Osteoporosis
Transcript
Learn about bone density, osteoporosis, and bone health issues that occur with aging.
DOCTOR: We’re here to discuss the results of your bone density scan, also called a DXA Scan.
A DXA Scan is a test to measure your bone mineral density. During DXA two different levels of x-ray energy are aimed at your bones in a process called scanning. The amount of energy absorbed by the bones is measured. This measurement gives us an idea of the density or amount of bone. The amount of bone that you have is then compared to the average bone density of other people the same age and gender. This measurement unit is called a z-score. When the measurement is compared to the average bone density of young adults of the same gender the measurement is called a t-score. DXA is simple, easy, non-invasive and painless. The bone area being scanned is placed between an x-ray generator machine and a receiver that records how much x-ray energy gets absorbed by your bone. Typically, your lower spine and/or hips are imaged but sometimes your wrist or the entire skeleton will also be scanned.
DOCTOR: It appears that your bone density is lower than normal. This is your z-score and t-score. And here’s your score. It tells me you’re in the category for osteoporosis.
PATIENT: What does that mean?
DOCTOR: Well, the score are representations of bone density that we can use to track your treatment. However if you want to understand what is actually happening in our bones, it’s helpful to imagine that they are like a concrete wall. The thicker the wall the more weight and pressure it can support and the more likely it is to last a long time.
Bone mass refers to the quantity of concrete within your bones. Generally the more bone mass you have the lower the chance of breaking a bone. On the other hand, the smaller your bone mass the higher the chance of breaking a bone with even a small injury. Osteoporosis is a condition where the bone mass is reduced to the point where the bone can easy break. This concept is similar to that of a weakly constructed concrete wall that is more likely to collapse under excess pressure or weight. Diagnosis of osteoporosis can be made on DXA scan when the measured bone density is lower than a certain t-score level. When the bone density of an individual is at or below a t-score of -2.5 that person is diagnosed with osteoporosis and is considered to be at a higher fracture risk compared to others at his or her own age with higher bone density.
PATIENT: I’ve never had trouble with my bones before. Why now?
Our bone mass is like a retirement account. While we are young and through early adulthood we continue to gain bone mass, or (i.e. add to our retirement account,) until the peak in our early 30’s (also called peak bone gain). After that time, we slowly “withdraw” our bone reserves as we age. The bone mass we acquire during youth, like (same as the cash in our retirement account,) sustains us during our later years.
The more bone mass tharet tt is in the account at its peak, the longer it will take for aging related bone loss toslower the decline to a level that is associated with increased chance for fracture.. Likewise, starting with less bone in the account or earlier “retirement” can mean a less comfortable existence during the aging years.
DOCTOR: Many women lose bone density as they get older and enter menopause.
PATIENT: What does menopause have to do with it?
Ovarian function is important for bone gain and for bone loss. Menopause is a stage in a woman’s life when she loses her of ovarian function; menopause is followed by rapid bone loss ,(such as at natural menopause or following surgical loss of ovaries,) is followed by rapid bone loss. Women can lose up to 20% of their bone within the first 5 years following menopause. The average age at natural menopause is 51 years.
With early menopause (at age before 45, occurring Entering menopause at an earlier age either naturally or after surgical loss of ovaries), women start losing bone at a younger age (early retirement). Premature menopause (at age <40) may even also shorten the period of bone gain. Menopause before age 45 is recognized as a fracture risk. Starting with less bone in the account or earlier “retirement” can mean a less comfortable existence during the aging years. Menopause before age 45 is recognized as a fracture risk.
Aging also itself is accompanied by changes in the building blocks that make up our bones. Even with the exact same bone mass, the skeleton of older people is more likely to fracture from the same degree of trauma compared to the skeleton of a young person. This tells us that both the quality as well as quantity of bone is important in determining fracture risk for any individual.
PATIENT: So what is a fFracture risk? What do you mean?
Fracture risk is the likelihood or “chance” of breaking a bone. Each woman’s risk of breaking a bone during her life is influenced by a number of factors including her genetic background, (which can to varying degrees influences both bone quality and bone quantity), her peak bone mass, her overall health, (such as loss in bone mass, reduced bone gain and worsening of bone quality due to can all be seen with different diseases,) menopausal status and age at menopause, degree and rapidity of bone loss after menopause, and her genetic predisposition. Your fracture risk can be calculated by looking at these factors plus lifestyle choices, such as smoking and use of certain medicines.
PATIENT: What can be done about reducing this risk for fracture?
DOCTOR: Some of the factors that influence your fracture risk are fixed and cannot be changed, like your genetic predisposition, your age and the age you enter menopause. Other factors you are able to alter using simple strategies such as regular physical activity, healthy eating habits and avoidance of smoking and alcohol, all of which can improve the quality as well as quantity of your bones. Lifestyle changes can go a long way in improving bone health and in lowering risk for bone fracture.
PATIENT: My mom takes a pill to help with her bone density. Should I be on medication now, too?
A variety of prescription treatments are available to reduce fracture risk. The timing of starting prescription treatment and the choice of treatment needs to be individualized based on the woman’s health profile and fracture risk severity.
Bones are constantly being built and rebuilt, a process called remodeling. The key players that are responsible for bone remodeling are two types of bone cells: osteoblasts, or (these are the “builders”,) and osteoclasts, or (these are the “demolition squad”.). Healthy bones are the result of a fine balancing act between the bone building and bone destroying cell functions. Prescription medicines for osteoporosis work to either help build bone by acting on the “builders”, an (anabolic agent), or prevent bone loss by targeting the “destroyers” an (antiresorptive agent).
Bisphosphonates are one group of prescription medicines that are commonly used to reduce fracture risk in women with osteoporosis. This class of medicines acts by slowing the bone destroying cells, (aantiresorptive effect), while allowing the bone forming cells (osteoblasts) to continue to build new bone; the net result is a slowing down of bone loss and net bone gain with improved bone density and therefore reduced fracture risk. As with all medicines, there are possible risks and side effects of this class of medicines. Stomach irritability is a common side effect related to taking these medicines by mouth. Prolonged use of this group of medicines (for well more than 5 years) can very rarely be associated with some unique risks, (such as atypical fractures and osteonecrosis of the jaw).
Anabolic medicines can help rebuild bone by improving the function of the bone forming cells, thereby increasing new bone formation.
For the otherwise healthy women who are experiencing bothersome menopausal symptoms, menopausal hormone therapy offers a dual benefit of providing symptom control as well as slowing down the bone loss (antiresorptive effect) that would otherwise be accelerated at the time of menopause.
Other medicines are available and new medications are becoming available that show promise to improve bone health without some of the issues associated with other hormone medications.
You should discuss with your healthcare provider which approach is right for you.
DOCTOR: The decision to start medical treatment and the choice of medicine for fracture risk reduction depends on your overall fracture risk (as assessed from a combination of your DXA result as well as any additional risk factors) and your unique health profile.
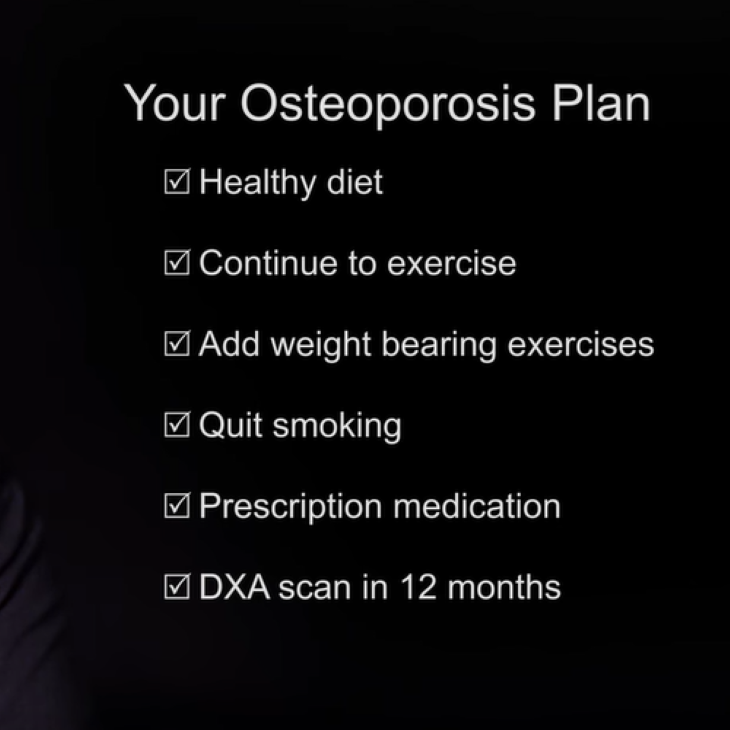
DOCTOR: Let’s review the plan:
- Continue to eat a wide variety of healthy foods, including leafy greens and milk to make sure you get enough calcium.
- Continue your walking program for exercise and add light weight lifting 2x/week.
- Work on quitting smoking.
- Based on your bone density result, your family history, and your age, you are at an increased risk for fracture and will benefit from prescription medication. Based on your risk and your overall health profile, the bisphosphonate class of medicines seems an appropriate choice.
- Check another DXA scan in 12 months; we hope that your bone density will remain stable or even improves after 1 year use of the prescribed treatment. In the event that you continue to lose bone mass further decline in your bone density is seen despite 1 year of regular treatment, further evaluation and even alternative treatment options may be considered.
PATIENT: Sounds like a great plan, thank you!
Menopause
Reproductive Aging
Find a Health Professional