What Is A Gestational Carrier & Who Needs One?
This SART micro-video will explain the aspects of using a gestational carrier including selection, screening, and indications.
Transcript
This SART micro-video will explain the aspects of using a gestational carrier including selection, screening, and indications.
Hello my name is Dr Mark Trolice. I am the director of fertility care of the IVF Center in Orlando Florida, and also the associate professor at the University of Central Florida College of Medicine. It is my pleasure to present our topic "what is a gestational carrier and who needs one."
The field of assisted reproductive technology or ART involves the addition of sperm to eggs in the embryology laboratory, then transfer of a select number of embryos to a woman's uterus. While traditionally the eggs and sperm have originated from a couple in a relationship, and the embryo transfer occurs in the woman who provides the eggs, ART has developed variations to accommodate patients' unique circumstances which may involve egg donation, sperm donation, embryo donation, and a gestational carrier. This micro-video will explain the aspects of using a gestational carrier including selection, screening, and indications.
There is an important distinction in the area of surrogacy, mainly whose eggs will be used. If a woman uses her own eggs and carries the pregnancy, she is called a traditional surrogate. However, if an intended parent (IP) provides eggs to another woman to carry the pregnancy, this woman is called a gestational carrier or (GC). In the United States GC Cycles are typically the only type performed with rare exception.
The process of GC requires a multidisciplinary approach. The team involves:
- a reproductive endocrinology and infertility specialist, well-experienced in third party reproduction,
- an embryologist who's well-trained in all aspects of in vitro fertilization or IVF,
- a mental health professional who specializes in human reproduction and who fully understands this unique form of parenting so intended parents and the GC can be appropriately educated and prepared, and
- a reproductive health attorney who has vast experience in reproductive issues not only state and national but depending on the circumstances, international, in order to protect the rights of all parties involved.
There are certain indications for using a gestational carrier. In addition to an absent uterus, either congenital, which means you were born with, or from surgery, abnormalities of the uterus that compell the use of a GC includes severe intrauterine scarring called Asherman's syndrome and multiple benign tumors of the uterus called fibroids - and that would be based on the fibroids location, size, and the woman's surgical history. Other conditions where a GC is recommended involve medical and biological contraindications to carrying a pregnancy where the woman or baby's life would be at risk, such as a condition called Pulmonary hypertension. Turner's Syndrome is a condition that would require egg donation because she does not make eggs and it's a relative contraindication to carrying a pregnancy and would also require a maternal fetal medicine or high-risk obstetrician, and pre-conception consultation if the intended parent wanted to carry the pregnancy. Other circumstances to use a GC include a single male, or in the LGBTQ population of a gay male couple, or single transgender female. Lastly, there may be a strong consideration for a GC if the woman has undergone multiple uterine surgeries for example, fibroid tumors, and also cesarean sections, where the uterine muscle may be weakened to result in complications near the end of the pregnancy as well as when recurrent miscarriage is unexplained following a thorough evaluation and multiple treatments.
What are the qualifications to be a GC? The standard criteria is a healthy woman with at least one prior uncomplicated pregnancy resulting in a live-born term delivery. However, it is advised that the GC not have more than five prior deliveries including three cesarean sections. A GC can certainly be a family member or a friend, but non-coercive informed consent must be assured. Or you can contract a GC independently or through an agency.
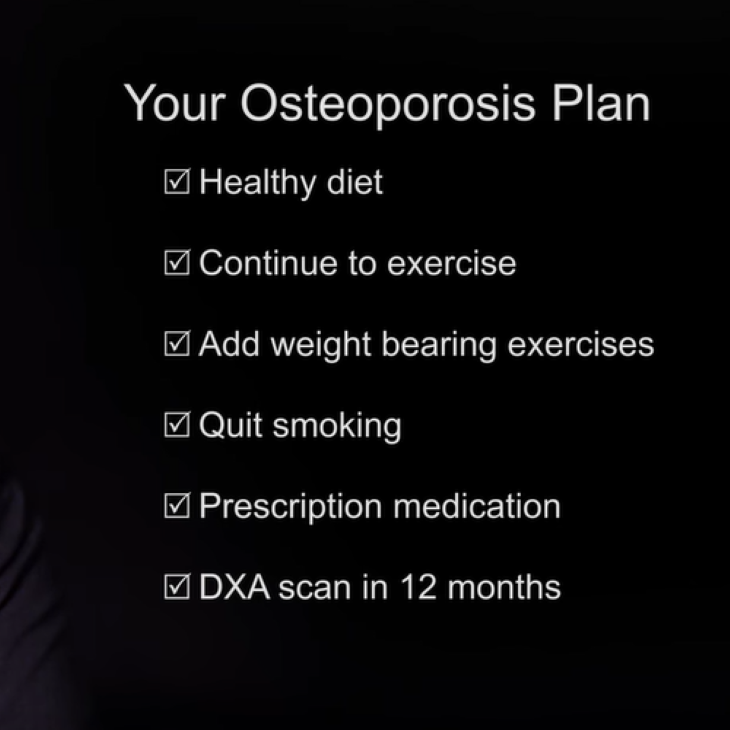
We typically prefer the GC to be between the ages 21-45, though most clinics recommend less than age 40 due to increasing pregnancy complications as a woman ages. The recoommended pre-cycle screening of intended parents or IPs who donate eggs and/or sperm and GCs is presented in the table below.
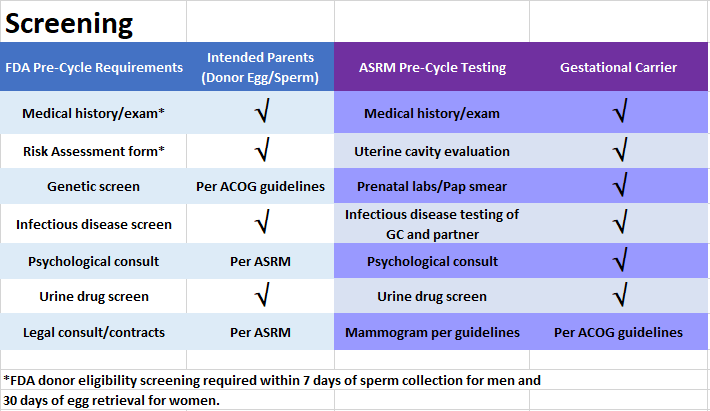
Both parties undergo a medical history, physical examination, psychological evaluation and counseling, as well as legal contracts. Essentially, all parties undergo the same testing with the exception of genetic screening of the GCs because there is no biological inheritance to the baby from the GC. The GC does undergo a urine drug screen and must have a prior uncomplicated term birth as mentioned. Additionally, the genetic IPs are required by the FDA to undergo infectious disease testing which involves screening for HIV, hepatitis B & C, syphilis, chlamydia, gonorrhea, plus a virus called cytomegalovirus, if the male will be a genetic parent.
Prior to the GC embryo transfer cycle, several procedures are necessary to increase the chances for a successful outcome. The uterine cavity should be evaluated either by a saline infusion sonogram or hysteroscopy procedure. At the same time, a mock embryo transfer can be performed using a catheter, similar to the one on the day of the real embryo transfer, and passing through the cervix into the uterine cavity to provide information to the doctor regarding the ease of transfer of the embryos and measurement of the distance to inside the top of the uterus. This allows preparation to accommodate a potentially difficult embryo transfer, as well as a guide to how far to insert the catheter into the uterus. The measurement has become less important as most embryo transfers are now performed under ultrasound guidance which can determine the appropriate placement of the embryos. For fresh egg donation cycles, stimulation of the IP or egg donor is done with injectable fertility medication for multiple egg development followed by egg retrieval and sperm insemination. For frozen egg donation cycles, the eggs are thawed, then inseminated with sperm. With either option, the GC's uterine lining will be synchronized with embryo development to optimize implantation.
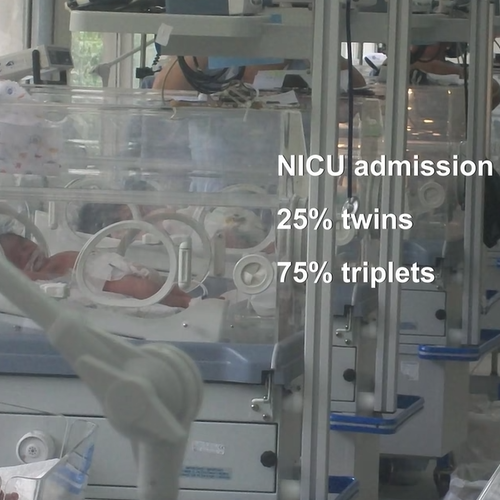
Finally, ASRM guidelines for the number of embryos to transfer should be adhered to and are typically based on the age of the woman who provided the eggs and the day of embryo development. A reproductive health attorney is a vital part of any GC arrangement. Consequently, separate legal counsel for the GC and intended parents is necessary to negotiate details of the contract. Contracts include but are not limited to financial obligations, expected behavior of the carrier to ensure healthy preganancy, medical procedures, and all legal matters, and creation of birth certificate. Laws vary among states in the U.S. and even among counties, as well as other countries, regarding the legalities of using a GC.
Third-party reproduction offers the opportunity of parenthood through a GC and without using the traditional biological mother's uterus. As third-party reproduction is more widely used, there continues to be a broader understanding of the ethical, moral, and legal issues involved. The goal of the provider and entire team of nurses, psychologists, agency, and attorney, is to facilitate the journey while maximizing a successful outcome for the intended parents. We hope this micro-video was educational and thank you for your attention. Please visit sart.org for all your questions on using a GC as well as all aspects of assisted reproductive technologies.
Gestational Carrier or Surrogacy
Find a Health Professional