Perimenopause
Transcript
This video will cover perimenopause, also known as menopause transition, including the changes you can expect and the treatments for symptoms that are available.
DOCTOR: How are you doing since our last yearly visit? When was your last menstrual period?
PATIENT: Lately they have been irregular, sometimes fewer days between periods....sometimes more than expected. I used to have regular 26-28 day cycles but recently they've been anywhere from 20 to 50 days in between. Plus, sometimes my periods are heavy and sometimes just spotting.
DOCTOR: Are you having any hot flashes, night sweats, or trouble sleeping?
PATIENT: What’s a hot flash?
DOCTOR: Hot flashes (also called hot flushes) are when a woman experiences a sudden feeling of intense heat, that may be accompanied by rapid heartbeat, and sweating. These events can be 2 to 30 minutes long, are unrelated to physical activity, and are the result of hormone shifts. They are a common symptom during the menopausal transition.
PATIENT: Sometimes I get hot all of the sudden, and I’ve been waking up during the night sometimes for no reason.
DOCTOR: Are you having any other symptoms?
PATIENT: Symptoms of what?
DOCTOR: Menopause transition.
PATIENT: I don’t know, what is menopause, exactly and what does menopause transition mean?
DOCTOR: Menopause is a normal stage in a woman’s life that marks the end of her reproductive years. It is defined by eventual and permanent stoppage of menstrual periods. Menopause transition, also called perimenopause, is the time period around menopause that can range from months up to a few years.
PATIENT: Oh. Like what kinds of other symptoms?
DOCTOR: Menopause transition can show up in lots of symptoms. Have you noticed having vaginal dryness particularly during sex? Do you feel tired or are you feeling depressed? Have you noticed any recent changes in your hair or skin or any problems urinating, or even trouble with your memory??
The symptoms of menopause transition are a result of the hormone levels that change as a woman gets older, and as her ovarian function declines and then eventually stops. The first symptoms women notice usually include changes in menstrual bleeding pattern, her cycles may shorten, lengthen or become irregular. She may also experience hot flashes, night sweats (when hot flashes occur during the night and are accompanied by sweating) and frequent nighttime awakening (usually due to episodes of night sweats). Trouble sleeping is soon followed by daytime fatigue, and forgetfulness. Symptoms of vaginal dryness are common and many women experience a decrease in sex drive around this time. As a woman moves further into menopause, she may also notice weight gain, problems with urination (such as urinary leakage) and even experience depression.
DOCTOR: I think you might be entering the period of transition to menopause that we call “perimenopause.”
PATIENT: What?, I’m still having periods, and I remember my mother being much older.
DOCTOR: Perimenopause is the transition from your fertile years towards menopause. It can even take up to 10 years…It’s really a process, not a single event.
PATIENT: Are you sure? 47 seems early. Is there a test for perimenopause?
DOCTOR: Every woman is unique, but most begin seeing changes like yours in their late 40s. The average age for menopause is 51. Getting a blood test right now won’t tell us much, because your hormone levels are changing frequently right now.
Hormone changes during perimenopause
To understand some of the symptoms of perimenopause including the changes infertility during this time, it’s important to understand the hormonal changes that happen as a woman gets older.
A girl is born with a large number of eggs, in her ovaries. Each egg lies within a tiny “cyst like structure” called a “follicle”. During a woman’s reproductive life, these follicles are the “hormone producing machinery” in her ovaries. Hormones produced by the ovarian follicles include estrogen and progesterone as well as additional hormones called inhibins and antimüllerian hormone or AMH. Ovarian production of estrogen in turn is controlled by a hormone called follicle stimulating hormone (FSH) that is produced by the pituitary gland in the brain.
From birth onwards, there is a progressive decline in the number of eggs and follicles in a woman’s ovaries throughout her childhood and reproductive years, until she reaches menopause when her ovaries are almost entirely depleted of follicles. With aging, as increasing numbers of eggs and follicles within the ovaries die off, levels of ovarian hormones drop. Each ovarian hormone, including estrogen, progesterone, inhibin, and antimüllerian hormone is has its own effect. This decline in ovarian estrogen levels is responsible for many of the symptoms of menopause transition such as hot flushes, night sweats, and vaginal dryness. Progesterone, a hormone which is high after ovulation-release of an egg, also may not reach as high a level during the menopause transition as during earlier reproductive years. In some cases, progesterone levels may not rise at all during a menstrual cycle. In those months, no ovulation occurs, leading to a missed menstrual period. Unlike blood levels of ovarian estrogen and progesterone which may fluctuate during the perimenopause, AMH and inhibin levels tend to steadily decrease over time during the menopause transition and actually become undetectable a few years before onset of menopause. The decline in inhibin and AMH levels is mirrored by rising blood levels of follicle stimulating hormone, or FSH, as the body attempts stimulate growth of remaining ovarian follicles.
PATIENT: If you know all these hormone levels change, why can’t you just measure the levels in my blood now to see where I am?
DOCTOR: Hormone changes vary from person to person and from minute to minute. So, while high levels of FSH and low levels of inhibin and AMH are well described during the transition period, there is no single and specific blood test that can be used to diagnose menopause transition. We use a combination of your age, personal and family history-particularly your menstrual history and presence of symptoms of menopause transition, as well as clinical exam to diagnose the menopause transition.
PATIENT: Seems like I have a lot to look forward to, how long is this perimenopause thing going to last? Are my hot flashes going to get worse?
Perimenopause or menopause transition can last from months to years. For any woman, it is difficult to predict how long her phase of transition will last before she becomes menopausal. Menopause officially starts when a woman has not had a menstrual period for a full year.
Whether a woman experiences symptoms of menopause and how severe the symptoms are varies from patient to patient. On average, women experience bothersome symptoms for about 4 years. But, for the majority of women, common symptoms such as hot flashes, night sweats, and sleep disturbances actually start to improve within a couple years of entering menopause. Other symptoms like vaginal dryness and urinary frequency may persist or even worsen with time. Decline in memory and skin changes are more reflective of the aging process than menopause per se. Most women’s fertility declines naturally long before the period of menopause transition. However, unplanned pregnancies can occur during this time and contraceptives should be used by those women who do not wish to become pregnant.
Hot flashes
Hot flashes are one of the most common complaints of women in the transition to menopause-- affecting almost two-thirds of women! These episodes produce a feeling of heat, flushing, redness and even sweating and are sometimes called vasomotor symptoms. They can happen occasionally, or, in a few women, occur so frequently that they are very bothersome and distracting. Fortunately, the frequency and severity of hot flashes decrease for the majority of women over the 5 years following their last menstrual period. But in a small percentage of menopausal women, hot flashes may persist for years.
Hot flashes are caused by fluctuations in a woman’s reproductive hormones and a decrease in the amount of estrogen produced in her ovaries. The good news is that there are a number of treatment strategies available to help with hot flashes. These include hormonal and many non-hormonal therapies that are commonly used to manage common conditions such as depression and high blood pressure. Many women find that lifestyle modifications such as weight loss, reducing their intake of caffeine, and stopping smoking can really reduce the severity and frequency of the hot flashes. Keeping the bedroom temperature cool, dressing in layers, and choosing sleepwear made of absorbent materials can also help. If frequent and persistent hot flashes are causing you discomfort, talk with your healthcare provider.
Occasionally severe, bothersome and persistent hot flushes may reflect a more serious underlying health concern. This is especially so for women who start having new symptoms after being menopausal for years.
Night sweats
A woman may wake up from sleep feeling hot or may wake up and find herself drenched in sweat, sometimes so much that she needs to change her clothing. Some women feel a sense of chill and cold on waking up. Night sweats are similar to hot flashes and for some women; they are more severe and bothersome. Like hot flashes, for the majority of women, both the severity and frequency of night sweats decline as a woman progresses into menopause. Night sweats are a common cause for poor sleep, and can contribute to symptoms of daytime fatigue, irritability and to symptoms of depression.
Skin and hair changes
Aging related changes in skin and hair are noticeable to almost all perimenopausal women. Increasing skin dryness, loss of elasticity, and worsening wrinkles are a part of aging, so it’s hard to know whether these changes are due to aging alone or because of a decline in ovarian hormones, particularly estrogen from the loss of ovarian function.
While some have suggested that taking menopausal hormone medications can reduce the skin changes with aging, there just aren’t reliable studies to show this is so. At this time, hormone therapy isn’t given just to help protect against skin aging. You can help reduce the pace of skin aging by avoiding excessive sun exposure, tanning beds, and smoking---things that are recognized as “skin insults.” Although there are many cosmetic products and interventions, many of which are costly, that claim to slow the appearance of physical signs of skin aging, it is impossible to determine which woman may benefit from what product.
Thinning of scalp hair and the appearance of stray facial hairs, especially on the chin and lip areas, are common complaints during this time. It’s not clear if these are due to hormone changes or aging per se. Studies of women taking menopausal hormone therapy haven’t shown any benefit of conventional menopause hormone therapy improve hair growth.
A woman’s genes seem to be the major factor in determining who may be at risk for scalp hair thinning.
A woman’s distress over changes in her physical appearance can be substantial.
This distress must not be simply dismissed as “vanity” since changes in skin and hair may reflect an underlying medical disorder such as thyroid disease or anemia. Scalp hair growth can improve with the use of Rogaine and hair follicle transplantation. Follicle transplant is a more permanent although costly solution when this problem is particularly bothersome.
Sexual desire
Women approaching menopause as well as those already in established menopause often report a loss of interest in having sex. These changes in sexual desire are commonly encountered in the women approaching menopause.
Menopause-related vaginal dryness and discomfort can diminish a woman’s sexual response and desire.. There are things that can help. Lubricants offer a quick, partial fix along with a partner who understands the situation. Other remedies include using a a vaginal moisturizer or vaginal estrogen, which is available in many forms such as cream, tablets and even a vaginal ring.
Poor sleep and fatigue can contribute to lack of desire and in this case, strategies that ensure restful sleep will translate into improved sexual wellbeing. In studies of women who were in menopause following the removal of one or both ovaries, low blood levels of ovarian hormones (particularly estrogen and testosterone) were found to play a role in decreased sexual desire. This was true in women who previously had no problems relating to sexual function and sexuality. For this situation, hormone therapy may be helpful. Sexual satisfaction is so important in helping sustain relationships and determining a couple’s wellbeing.
But problems and concerns about sexual function typically aren’t volunteered by women and men until the problem looms large in a relationship. Occasionally an underlying medical disorder may contribute to the picture, such as depression or thyroid dysfunction.
Depression
Depression symptoms tend to increase in women approaching, entering and progressing through the early menopausal years.
There are a number of reasons this can happen. The combination of life changes such as financial status, concerns about your aging parents, and kids moving away, as well as dissatisfying sexual encounters, deteriorating relationships, and even the loss of a spouse through divorce or death, physical changes with disturbed sleep, frequent and severe vasomotor symptoms, may each contribute to the overall psychological burden for women going through perimenopause.
It is important to know that menopause is NOT a cause of depression but rather sets the stage for other players to act out! Although a trial of menopausal hormones or antidepressant therapy may improve depressive symptoms in some women, psychological evaluation and counseling is helpful for most.
Those same strategies we’ve already discussed to improve the quality and quantity of sleep can also help with depressive symptoms as well as your overall quality of life
It’s thought that the decline in hormones produced by the ovary plays some role in the depressive symptoms encountered in early menopausal women. Some women find that their mood improves with menopausal hormone therapy. However, if depressive symptoms begin suddenly, they may be due to an underlying and undiagnosed medical condition such as thyroid dysfunction.
Memory deterioration
Increasing forgetfulness and lapse in short-term memory are common complaints of women in perimenopause. As with depression symptoms, a combination of factors including life experiences that necessitate a juggling act, disturbed sleep, physical and psychological distress may contribute to these changes in memory.
Unlike the hot flashes, night sweats, and vaginal dryness that clearly are symptoms of menopause, deterioration in memory CANNOT be solely attributed to the loss of ovarian function.
A decline in ovarian estrogen is thought to contribute to some short-term memory changes. However, using hormone therapy has not been shown to consistently make a lasting positive impact on memory in postmenopausal women.
What’s actually more concerning is that a few studies have suggested that using menopausal hormones in elderly women may even harm thought processing and memory. Aging itself is accompanied by changes in bodily function, and a number of diseases and disorders become more common as we grow older, including some that can contribute to memory loss (such as high blood pressure, stroke, and thyroid disease).
Vaginal dryness
Of all the symptoms related to aging and menopause, vaginal dryness is probably the one that many women are embarrassed to bring up. It is one that tends to increase with age and it is also one that can be successfully treated with very little treatment-related health risks.
Loss of ovarian estrogen is the major culprit. It results in thinning of the skin and tissue at the opening to the vagina and inside as well. Vaginal dryness typically starts before the onset of menopause and can worsen with time. A number of strategies are available to successfully address the problem of vaginal dryness. These include over-the-counter agents such as lubricants and moisturizers, as well as prescription hormone options.
Interrupted sleep
Many women find that sleeping becomes a challenge during perimenopause—they can’t fall asleep or can’t stay asleep, or both.
A number of treatment options can help. In addition to over-the-counter agents, hormonal therapies, and non-hormonal medications, strategies called sleep hygiene often improve both sleep quality and quantity. Sleep hygiene involves attention to the timing of sleep, and restricting distractions and stimuli before bedtime by avoiding use of TV, computers and electronic gadgets just before going to bed. Weight loss if you are obese, and exercise if you are sedentary, can also improve night sleep.
PATIENT: This description of perimenopause sounds miserable….will I have all of these problems? Can they be treated?
DOCTOR: Menopause transition is a normal phase of life and not a disorder. It is not bothersome for all women. Every woman’s experience is different. You may have several, all, or just one or two of these symptoms. The good news is that there are many different treatments to help. Women don’t need to suffer. Many of the symptoms of perimenopause are directly related to the falling levels of estrogen. So taking estrogen (available in various forms) can effectively address many of the symptoms. It is however important to appreciate that estrogen therapy may not be a good choice for everyone, and a number of alternative non hormonal options are available for the management of menopausal symptoms for these women who may not be good candidates for estrogen therapy.
For those considered good candidates to try menopausal hormones for symptom management, the type of hormonal treatment needs to be tailored to the individual. For instance, a woman who has had her uterus removed can take estrogen by itself. But a woman who still has her uterus will also need to take progesterone or an alternative medication to protect her uterus.
The method of hormone delivery can depend on what symptoms the medicine is being taken to relieve. For help with vaginal dryness or urinary frequency, placing the estrogen directly in the vagina as cream or tablet or vaginal ring is preferred. For management of hot flashes and night sweats, taking estrogen either by mouth or across the skin as a patch, gel or spray is more effective and preferred.
PATIENT: My sister uses hormones specially made for her from a compounding pharmacy….are those better?
DOCTOR: Compounded hormones are made by a local pharmacist, sometimes individually for a patient. It is important to recognize that they are not monitored by the FDA and there are concerns about batch-to-batch variation.
Commercially produced bioidentical hormones are regulated by the FDA for safety, efficacy (effectiveness), side effects, and content. They are held to the same safety standards as all regulated medicine. Compounded hormones are considered health supplements for regulatory (not safety) purposes. FDA regulations require packaging to warn the consumer about risks, contraindications (situations where the medicine should not be used), and purity of the product. Compounded hormones are not required to provide this information and are specific to the individual patient’s medical history.
Dosage (over- or underdosing) and absorption of hormones may determine the safety of the product. Dosage and absorption information are not available for compounded medications. So a woman may not receive the dose of hormone she believes is in her medicine. Some compounded hormones are not found naturally in the human body and so their effect, risks, and benefits are unknown. Unlike commercially available bioidentical hormones, compounded hormone formulations are not monitored by the FDA, so safety information is largely unknown.
PATIENT: Are compounded bioidentical hormones more effective than commercially available formulations?
DOCTOR: There is no medical evidence to suggest that compounded hormones are more effective than commercially available bioidentical hormones. Customized compounded hormone regimens may add additional health risks due to lack of safety information, variable absorption, and variable purity. Individualized hormone preparations are not more effective than standard hormone preparations, regardless of blood, urine, or saliva testing of individual hormone values.
DOCTOR: The next thing we should talk about is what you’re using for birth control.
PATIENT: Oh, well, is that still a problem? We’ve been using condoms. Do I still need to use birth control?
DOCTOR: During perimenopause, the chance of getting pregnant does go down, but you CAN still get pregnant. Actually, some types of birth control may even help with some of your symptoms.
Birth control pills, particularly including those containing hormones that are similar to ovarian estrogen and progesterone (combination pill) may help in the same way as conventional hormone therapy. Since the dose of hormones in birth control pills is much higher than in conventional menopausal hormone therapy, low dose formulations are recommended to minimize hormone use related risks (such as of clots and stroke) when choosing a birth control pill for a woman in the menopause transition.
A vaginal ring or an IUD can be another good method of birth control. Besides preventing pregnancy, the vaginal ring contains hormones that can alleviate some symptoms of menopause. A progesterone-containing IUD, in addition to being a highly effective contraceptive, offers the benefit of improving heavy menstrual flow, but will not be of any benefit for other symptoms such as hot flushes. Hormonal contraceptives can be used safely until the time of menopause.
Barrier methods of birth control such as a diaphragm or condoms will prevent pregnancy, but won’t help with menopausal symptoms.
For an otherwise healthy, non-obese, active perimenopausal woman who is a non-smoker, and who does not have any history of stroke, clot or of early onset heart disease in a close relative, a low dose combination pill may be a safe and effective strategy that provides a dual benefit of contraception and symptom control.
PATIENT: Is there anything else I need to know? What else should I be thinking about now that I’m approaching menopause?
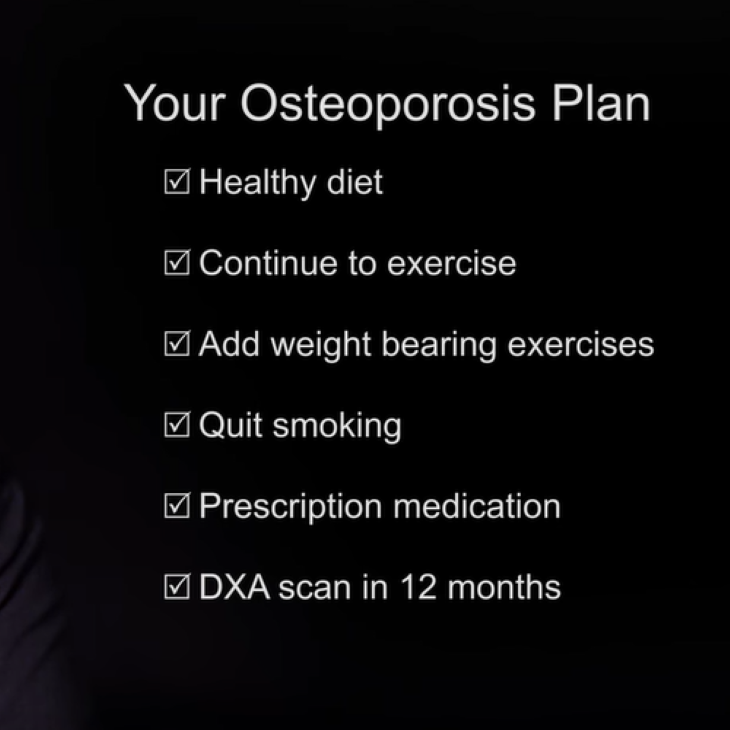
DOCTOR: This is a great time to start working to keep your bones healthy. As menopause approaches and ovarian hormone production falls, bone density also goes down and the risk for osteoporosis goes up.
Our bones can be compared to a concrete wall – the thicker the wall the more likely it is to sustain heavier loads and pressures, and the more likely it is to last for a long time. Bone density or bone mass refers to the quantity of ‘concrete” within our bones. Basically, the more bone mass a woman has, the lower her chance for fracture.
The flip side is also true, the less bone mass a woman has, the higher her chance of breaking a bone with little trauma. Regular weight-bearing exercise can increase bone strength. It’s important to make sure you have enough calcium and vitamin D on board to keep your bones healthy. Supplements might be a good idea for you particularly if you don’t get enough in your diet.
DOCTOR: Once you reach 65, we’ll do a bone density screening. It’s not needed now; you don’t have any of the risk factors for fracture risk such as personal history of fracture or arthritis, low body weight, or use of certain medications that can affect the skeleton, such as oral glucocorticoids (such as steroids) or family history of osteoporosis or of hip fracture.
For otherwise healthy women who are experiencing bothersome menopausal symptoms, hormone therapy can offer a dual benefit of providing symptom control as well as of slowing down the bone loss that would otherwise be accelerated at the time of menopause. Simple strategies such as regular physical activity, healthy eating habits and avoiding smoking and alcohol go a long way in improving bone health and in lowering risk for bone fracture.
DOCTOR: We’ve covered a lot today….let’s go over your plan.
- Start taking low dose birth control pills prescribed today. Those should help with birth control as well as decrease some of your symptoms. Plus, your periods will be more regular and less heavy.
- Get started with a regular walking plan. You might also look into starting regular exercise regimen that includes weight bearing sessions.
- We have talked about optimizing your intake of calcium and vitamin D, aiming for a daily total intake of 1000mg of calcium and 600IU of vitamin D through a combination of diet and supplements.
- Start keeping a symptom chart as this information will help us to identify the severity of your symptoms as well as help gauge the benefit from recommended treatment and lifestyle changes.
- Understand that these are normal and natural changes, and we’re here to help. Let’s check back in a few months’ time to see how it’s going. If you have any concerns before our next visit, please feel free to touch base with me.
Menopause
Abnormal Uterine Bleeding
Reproductive Aging
Contraception
Find a Health Professional