Male Fertility and Infertility
Transcript
This video was created to provide information on male factor infertility and its treatment.
MD: What brings you here today?
Couple: We haven’t been able to get pregnant..
MD: Tell me more about that.
Couple: What do you want to know?
MD: How long have you been trying and when was the last time you used birth control? How often do you have sex? Do you have regular menstrual periods?
Couple: Well, we’ve been trying to have children for awhile now…. (fade off as talks)
MD: It seems like you’re having regular periods and ovulating, are you ready to talk about the next steps?
Couple: Yes- absolutely, we’re anxious to get our family started.
MD: Well, the good news is that your [MD looks at wife] periods are regular and you seem to be ovulating without any problem. Now we need to look for other reasons that may be keeping you from getting pregnant.
Couple: Like what?
MD: Let’s take a two-pronged approach and look for issues with both you and your husband.
Husband: So I might be the problem?
MD: About half of all infertility is due to the male partner in whole or in part. Were you aware of that?
Husband: I guess I thought if I was making sperm, everything on my side was fine.
MD: Actually, to be fertile, a man must produce enough sperm, and ones that are able to fertilize an egg.
Husband: Isn’t one sperm enough?
MD: It’s true that only one sperm fertilizes the egg, but millions of sperm are usually needed to give a good chance of that happening. Presence, quantity, quality, and getting the sperm in contact with the egg are all important.
When a boy goes through puberty, the same hormones that are responsible for muscle growth, facial hair, and deepened voice also trigger the production of sperm in the testicles (testes). Men produce sperm throughout their lives, though the number of sperm produced tends to decrease after age 50 or so.
Sperm quality:
It’s not enough to make sperm; the sperm that is produced must be of good quality in order for a pregnancy to happen.
Husband: What do you mean, quality?
MD: Delivery is the next step and is a longer process than you may realize. Did you know that each sperm takes 3 months to fully mature?
Husband: (Looks at wife, puzzled)
MD: Delivery includes a few phases: moving sperm through the maturation process, ejaculation, and getting the sperm to the egg so it can be fertilized.
Immature sperm (spermatogonia) are produced in the testes and travel into the epididymis where they mature and are stored until they are released with ejaculation.
In order to conceive naturally, sperm must be released during orgasm (ejaculated). When a man is sexually aroused, his penis gets larger and stiffens. During orgasm, mature sperm mixes with fluid produced by other nearby glands called the seminal vesicles, prostate, and seminiferous tubules.
This mixture is called semen and travels through the urethra and exits the opening of the penis. A typical ejaculation contains at least 15 million sperm in each milliliter of semen and can vary in volume from about a quarter teaspoon to a teaspoon (5ml). Each ejaculation typically contains 40-75 million sperm.
Finally, sperm must come into contact with an egg in order for a pregnancy to occur. This usually means having sex with ejaculation around the time a woman ovulates (releases an egg). The 5 days before and up to the day of ovulation is sometimes called the “fertile window.”
Couple: Well, all that seems to be working fine. Why test that?
MD: Since about half of couples with infertility have some male factor involved, it’s a good place to start. We would like to do a complete evaluation.
Husband: Ok, but what are do you need from me?
MD: Remember what needs to happen for successful reproduction? Your workup will help us find out about whether you’re making enough sperm of good quality and whether it’s getting where it needs to go.
First we will do a detailed history.
Here are some specific examples of things you might be asked about and the reasons for those questions.
Fever: A high fever can harm the function of the testicles and the sperm. The effects of a fever on sperm can last for up to 2-3 months after the illness, so pinning down the timing is important.
Childhood diseases: For instance, a man who had mumps, especially after puberty, may have a low sperm count as a result of the swelling of the testicular tissues during the illness.
Undescended testicle: Some baby boys are born with one or both testicles still inside the abdomen rather than down in the scrotum. Having undescended testicles (cryptorchidism) can cause problems with sperm production. About 30% of men with one undescended testicle and half of men with two undescended testicles have a low sperm count.
The timing of puberty: Starting puberty late or having incomplete puberty may reveal a hormone disorder. The timing of puberty and other specific signs such as how often a man needs to shave can give important clues to a man’s hormone function.
Respiratory illness: Certain symptoms and diseases that have no obvious connection to reproduction, such as repeated respiratory infections and cystic fibrosis, can be associated with impaired fertility.
Infections: Some conditions can cause scarring and/or blockage of the reproductive tract. This can prevent the normal ejaculation of semen. Sexually transmitted infection, infection in the epididymis, and prostate infection are three conditions that should be explored.
Surgery: Past surgeries are another crucial part of the history. Having had bladder, pelvic, or retroperitoneal surgery or a spinal cord injury can contribute to ejaculatory dysfunction.
Trauma: Injury, due to direct trauma to the testicle, can result in problems with sperm production. Having had testicular torsion, which is a twisting of the testicle, may also damage the testicles, even if surgery was not needed.
Sexual history: Questions about the frequency of sex, sexual behaviors, method of intercourse, and any problems with sexual function are important in the workup of male infertility. Correct timing of intercourse with the female partner’s ovulatory cycle can be crucial in getting pregnant. Since sperm can reside in the woman’s reproductive tract 1-2 days after intercourse, having sex about every 24-48 hours around the time of ovulation can improve a couple’s odds of conception.
Lubricant use: Did you know that many sexual lubricants such as petroleum jelly and even water-based lubricants can reduce sperm motility and should be avoided? Using a special lubricant that does not interfere with sperm is recommended. For example, you can use canola oil or mineral oil. Also, lubricants that are specially designed not to interfere with sperm are available on the internet. Check with your fertility specialist to help decide which is the right lubricant for you.
Men who are infertile may also have other health problems. In fact, 1%–6% of men who seek treatment for infertility have significant medical problems even when they have a so-called “normal” semen analyses.
Research shows that more than 1 out of 5 men being evaluated for infertility are found to have depression and erectile dysfunction. Infertility and semen production problems have also been linked to hormonal disorders, cancer, and higher risk of early death in later years.
Exposure to chemicals/toxins: Exposures to environmental or industrial toxins as well as any medications should be discussed as these can affect male fertility. Some medications can decrease the production of male sex hormones (androgens). Common antibiotics can temporarily affect sperm formation. Many chemotherapy treatments harm sperm formation. Some common medications for high blood pressure and depression may affect a man’s ability to ejaculate.
Drug/Tobacco/Alcohol use: Recreational drug use can also have a significant impact on male fertility. Cigarette smoking can affect sperm number, motility, and shape. Opiate use affects normal hormone secretion by the pituitary and can affect testicular function and lower testosterone levels.
Steroid use: Anabolic steroid use can also impact male fertility. These male hormone drugs are known to stop the normal interactions between the hormone control center in the brain (hypothalamus and pituitary) and the testicles. As a result, less testosterone and sperm are produced by the testicles. Men who take anabolic steroids often have very few or even no sperm.
Use of testosterone: Men with low testosterone should not use testosterone gel or injections while trying to conceive. Using a testosterone supplement may cause a man’s sperm count to drop.
Hot tub/Sauna use: Exposure of the testicles to too much heat can damage sperm production (spermatogenesis). The harmful effects of using a hot tub or sauna can last for up to three months. In today’s digital age, laptop use has been shown to increase scrotal temperature, although no data exist to show this harms sperm production or fertility.
Couple: After the history, then what?
MD: Once the history is complete, a physical exam will be done… and not just on your private parts. I will do a complete physical exam, checking your head, neck, chest, genitals, and extremities for clues that might mean you have a hormonal imbalance or other conditions that can affect sperm.
You will be asked to stand so that your scrotum can be checked. The clinician will gently feel each testicle and check their size and firmness. Volume and size are important. A smaller or softer than normal testicle can suggest a problem with sperm production. A mass in the testicles may mean there is cancer present.
The scrotum will be checked for a varicocele. This is swelling and engorgement of a complex group of blood vessels near the testicles. Bearing down can make the varicocele larger and easier to feel. Nearly all varicoceles are found on either the left side or both sides (>90%).
Other parts of the scrotum are checked as well. Hardened areas, tenderness, or cysts may mean a blockage, called an obstruction. It’s also important for the clinician to check the presence or absence of the vas deferens, the ducts through which sperm travel during ejaculation. Approximately 2% of infertile men are born without these ducts, called congenital absence of the vas deferens (CAVD). This condition is also associated with having the gene for the respiratory disease known as cystic fibrosis.
The clinician will check your penis for any abnormalities that might cause a problem in getting sperm to the back of the woman’s vagina during intercourse.
MD: The next step is the semen analysis. This will tell us if there are enough sperm that move and are shaped normally.
Couple: What all is involved?
Husband: What are you looking for?
MD: Among other things, we measure the amount of semen you produced, the number of sperm, , how many are moving, and how many of the sperm are shaped normally.
Husband: I’m not sure I can produce a sample on demand. It sounds embarrassing.
MD: We have a nurse who will walk you through the process and answer your questions before you get started. You will have privacy and materials to help you if you want them. We might even be able to let you collect your sample at home and bring it to us if you live a short distance away.
Sometimes, other specialized tests will be done if needed.
In some men, semen can flow into the bladder. This can be seen by collecting a urine sample immediately after ejaculation for men with low semen volumes and low numbers or absence of sperm.
It may be helpful to check hormone levels, such as follicle stimulating hormone, testosterone and luteinizing hormone. About 3% of infertile men have a hormone disorder. High hormone levels can result in very low production of sperm or even no sperm. Low hormone levels can indicate congenital conditions or the use of anabolic steroids. High levels of the hormone prolactin (hyperprolactinemia) can be due to medications, illness, or a tumor in the pituitary gland in the brain.
Genetic Studies
Approximately 15% of infertile men with no sperm or very low sperm counts have a genetic abnormality that can be found through genetic testing. Some genetic abnormalities are known to have certain effects on reproduction. Genetic testing can give insight into whether a man with a given condition can father a child and what might need to be done to help that happen. It also can give information about the health of potential children, like in the case of cystic fibrosis.
Genes are parts of cells that contain information passed from parents to children. Researchers have identified small deletions in genes on the Y chromosome that are often found in men who produce little or no sperm. Blood tests can show these deletions and may be recommended for men with extremely low or no sperm. It is important for men to know if there are deletions because this can be passed on to sons. The type of deletion can also help predict what treatments could be successful.
Analysis of the chromosomes, called karyotyping, can also be helpful especially in evaluating men with severe low sperm counts or no sperm. For instance, Klinefelter syndrome, where a man has an extra X chromosome, is the most common genetic reason for having no sperm.
Couple: Once I know what the problem is, what can I do about it?
MD: Your treatment will address the specific problem you have.
Varicocelectomy
When a man with a varicocele has an abnormal semen analysis, pain in his testicle, and/or testicular atrophy (a testicle which has decreased in size), the varicocele can be repaired using surgery or other techniques. After treatment, many men see an improvement in their semen analysis.
Microsurgical Reconstruction for Vasectomy and other blockages
Each year approximately 500,000 men undergo vasectomy as a form of permanent contraception. Some later decide to have it reversed. Blockages from vasectomy or other causes such as infection or trauma sometimes can be surgically repaired.
Sperm Retrieval Techniques
Microsurgical Epididymal Sperm Aspiration (MESA) is a procedure to surgically remove sperm from the epididymis. Using an operating microscope, the tiny tubules of the epididymis are opened and sperm are retrieved. The sperm are either used immediately for a procedure called intracytoplasmic sperm injection (ICSI) along with IVF to fertilize an egg with these sperm or frozen (cryopreserved) for future use.
Testicular Sperm Extraction
(TESE)/Testicular Sperm Aspiration (TESA) are surgical procedures. In TESE, small pieces of testicle tissue are taken out (biopsied) and the sperm are collected from the tissue under a microscope. Only a small percentage of testicular sperm can swim on their own, although they are fully formed. ICSI with IVF is used to fertilize an egg with these sperm. TESA is similar to TESE except that no incision is made and instead a small needle is used to collect the sperm directly from the testicle.
Transurethral Resection of the Ejaculatory Ducts (TURED)
Blockage of the ejaculatory ducts is found in fewer than 5% of infertile men. TURED removes an obstruction in the ejaculatory duct and can improve sperm counts.
Other treatments involve assisted sperm collection:
When semen goes into a man’s bladder instead of coming out through the penis during ejaculation, medications that help close the bladder neck can be given and help with release of the sperm. For these men, sperm can also often be collected from his urine after he ejaculates.
Assisted Ejaculation
Some men are physically unable to ejaculate and can be helped with vibratory stimulation or electroejaculation (EEJ). These procedures can cause ejaculation using vibratory stimulation on the penis or stimulation of nerves in the rectum with an electrical probe.
Sometimes, treatment with medication can help with male infertility: Medical Treatment for Idiopathic Infertility
Medications are sometimes used to treat male infertility when there is no clear cause.
Clomiphene citrate is one of the most widely used drugs for treating low sperm count when a cause can’t be found. However, this is an off-label use, meaning that it is being used in a different way than described in the FDA-approved drug label. Also, studies of clomiphene have not clearly shown a benefit for this use.
Some studies support that antioxidant therapy (i.e., zinc, vitamin E, vitamin C, L-carnitine, N-acetylcysteine, etc.) may improve pregnancy and live birth rate in couples with male infertility, though these studies are small and inconclusive.
Couple: What if I find I have a problem with my sperm? What if we find we have female fertility problems too?
MD: Up to 30% of couples have issues with both the male and female partners, Sometimes, depending on the type of issue uncovered in the fertility evaluation, intrauterine insemination (IUI) or assisted reproductive techniques are used to help achieve pregnancy.
Couple: Assisted reproduction? Like IVF?
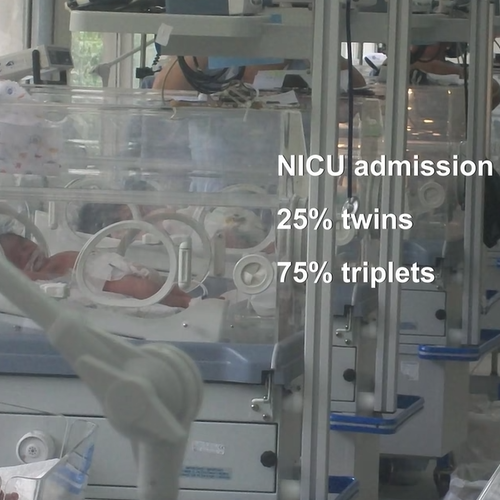
Assisted reproduction technologies (ART) include procedures where both eggs and sperm are handled outside the body. In general, ART involves surgically removing eggs from a woman's ovaries, combining them with sperm in the laboratory, and returning them to the woman's body or donating them to another woman.
ICSI is a procedure in which a single sperm is injected directly into an egg to fertilize it. It is often used for men with infertility along with IVF to increase the chance of pregnancy.
These techniques have allowed many infertile men to become biological fathers.
Each of these treatments comes with its own cost and risks. These will be explained to you by the treatment team to help you decide the best course of action to help you achieve your desired goals.
MD: Do you have any questions? Let’s schedule a physical exam for you with an urologist specializing in reproduction. We’ll meet again soon to discuss our next steps,
Couple: Thanks, doctor!
Infertility
Male Fertility/Andrology
Find a Health Professional