Fibroid Tumors
Transcript
An educational video that answers patient questions about the causes, symptoms, diagnosis and management of uterine fibroids. Developed by the American Society for Reproductive Medicine Patient Education Committee in cooperation with the ASRM Fibroid Special Interest Group.
A 37-year-old woman goes to her doctor for evaluation and treatment for infertility. She has never been able to get pregnant and very much wants to have a baby. She has bleeding for 10 days with her periods and she says she has feelings of fullness in her pelvis and pain during her period. Intercourse can be painful at times and she often battles constipation. During her physical examination, her doctor feels a large mass on her uterus and recommends further testing. An ultrasound shows a mass measuring 10 cm (about 4 inches) in diameter. The mass, which the doctor believes is a fibroid tumor, extends into the cavity of her uterus. Her doctor talks with her about several treatment options and she chooses to have a myomectomy. This procedure allows the tumor to be surgically removed from her uterus using a minimally-invasive technique. She recovers quite well and 3 months later, while completing some of the testing for infertility, she gets pregnant. She has no complications during her pregnancy and delivers a healthy girl at 9 months through a cesarean section.
This story is quite typical for many reproductive-aged women. Uterine fibroids are also called myomas or leiomyomas. These are benign tumors, meaning they are not cancerous. They are quite common and can affect between 30 and 50% of women of reproductive age. It is estimated that uterine fibroids will affect 8 in 10 African American women and 7 in 10 Caucasian women by menopause.
Let’s begin with some basic anatomy. The uterus is a muscular, hollow, pear-shaped organ that contains and nourishes the embryo and fetus from the time the fertilized egg is implanted to the time of birth of the fetus. It lies in the pelvic cavity between the bladder and the rectum. The nonpregnant uterus is approximately the size of a clenched fist.
There are two main parts of the uterus – the body and the cervix. The body has strong, muscular walls that expand during pregnancy. The cervix is the lower part of uterus that joins the vagina.
There are two main layers in the body of the uterus: the myometrium is the muscular wall forming the main mass of the uterus. The endometrium is the inner layer of the uterus that undergoes changes throughout the menstrual cycle.
Fibroids develop from genetic changes in a smooth muscle cell within the myometrium. The cell multiplies to form a tumor. The exact cause of uterine fibroids is unclear, but there is evidence that it may be a combination of both genetics and hormones.
Fibroid growth is regulated by many different factors, including hormones. Estrogen and progesterone (hormones produced primarily by the ovaries) may stimulate growth of the fibroids. And, after menopause, when hormone levels are low, fibroids rarely grow and frequently shrink. Maintaining a healthy diet and exercise seem to reduce the risk of fibroids. Medications such as low-dose birth control pills have little or no impact on fibroid growth.
Fibroids are usually found in or around the body of the uterus, but sometimes occur in the cervix. Fibroids within the uterus can be divided into three categories: subserous, located in the outer wall of the uterus; intramural, found in the muscular layers of the uterine wall; and submucous which can protrude into the uterine cavity (Figure 3). In addition, fibroids can be connected to the uterus through a stalk (called pedunculated). About 55% of fibroids are subserosal; 40% are intramural; 5% are submucosal. Fibroids are rarely found outside the pelvic cavity.
Symptoms from fibroids are related to their size and location. Although most women with fibroids have no symptoms, many may have significant symptoms, including pelvic and abdominal pressure or pain and excess bleeding. Approximately one-third of women with fibroids will have abnormal uterine bleeding, pain or pressure in the lower abdomen. Women with fibroids pushing into the cavity of the uterus often have irregular bleeding and may have problems with fertility. Fibroids in the muscle or just beneath the outer surface of the uterus are more likely to cause pressure, pain, and affect nearby organs, such as the bladder or rectum. This image shows a uterus with a large fibroid. Sometimes, fibroids can enlarge so much that they change the shape of the uterus.
Let’s discuss some of the common symptoms associated with fibroids.
Abnormal uterine bleeding is the most common symptom associated with fibroids and is the main reason women seek treatment. Intramural and submucosal fibroids can distort or enlarge the uterine cavity. Pressure from submucous fibroids on the endometrium can cause excessive bleeding. Because abnormal uterine bleeding can result from other causes, such as endometrial cancer and hormonal problems, it is important that women with fibroids who have abnormal vaginal bleeding receive a thorough evaluation for other causes of bleeding.
Pain is a common symptom of fibroids. Women with fibroids may have painful menstrual cramps.. A rapidly enlarging fibroid may outgrow its blood supply and degenerate, causing pain and cramping. Pedunculated fibroids, which are attached to the uterus by a thin stalk, may twist and cause severe pain. Large uterine fibroids, or those which push on the bowel, the vagina, or pelvic wall may also make bowel movements, sexual intercourse, or certain movements painful.
Large fibroids may press on nearby pelvic organs. If the fibroid presses on the bladder, which lies in front of the uterus, a woman may have urinary frequency or urgency as shown in the MRI image here. Pressure on the ureters, which are the tubes that transport urine from the kidneys to the bladder, can result in kidney damage if the fibroids are not removed. Fibroids in the lower uterus may put pressure on the large bowel and rectum, which could cause painful bowel movements, constipation, changes in the shape of stools, or hemorrhoids.
Fibroids may affect fertility and can impact pregnancy. Uterine fibroids are found in 5-10% of infertile women. However, fibroids are the single cause of infertility in only 2-3% of these women. So it’s important for infertile women and their partners to have a thorough investigation to identify other causes of infertility.
There are several explanations for why uterine fibroids may affect fertility:
- Changes in the position of the cervix (the vaginal opening to the womb) from the fibroids above may affect the number of sperm that can travel through the cervix.
- Changes in the shape of the uterus can interfere with sperm movement.
- Changes in the uterine muscle which prevents movement of the sperm or embryo.
- Inflammation in the wall of the uterine cavity which can affect implantation.
- Effects on the blood flow to the uterine cavity where the embryo would implant.
- Blockage of the fallopian tubes by the fibroids.
- The egg and tube are separated by fibroids and the egg cannot find its way into the tube.
If the fibroids are in the uterine cavity or push on the fallopian tubes, they can affect a woman’s fertility. However, it is not clear whether fibroids in the uterine muscle affect fertility if they do not directly influence the movement of sperm, egg, or embryo. In a study of women with unexplained infertility, the chance of pregnancy was 25% for a woman who did not have fibroids. For women with fibroids, the chance to get pregnant was 11%. In women who had fibroids but had them removed, their chance to conceive was 42%. This shows that fibroids may play a role in hampering a couple’s ability to conceive.
Fibroids that affect fertility are usually submucosal or intramural. With in vitro fertilization, a form of assisted reproductive technology, fibroids in these locations may also lower success. Fertility is affected because the fibroids either are within, or pushing into, the cavity. Large fibroids measuring 5 cm or greater also decrease the chances of success.
Fibroids may or may not grow during pregnancy or cause complications. If a fibroid does grow, it will typically do so in the first 12 weeks of pregnancy. It may also shrink later in pregnancy. This image shows a large fibroid pressing into the uterine cavity next to the developing fetus.
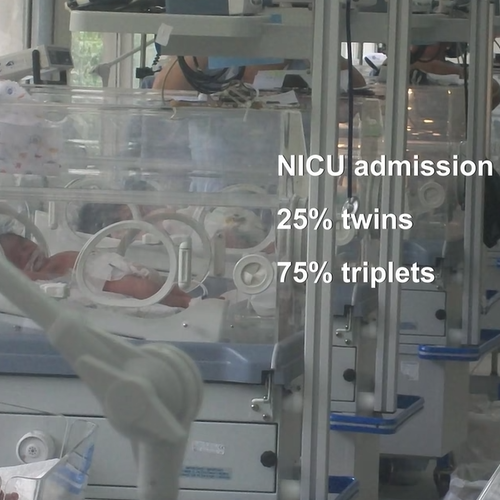
Sometimes when fibroids enlarge during pregnancy, they outgrow their blood supply and degenerate. However, fibroids that remain or grow can change the baby’s position, and increase the risk for Cesarean section, miscarriage, and preterm birth. The management of uterine fibroids depends on your physician’s recommendation. In certain cases, surgery to remove the fibroids prior to conception can reduce a woman’s chance of miscarriage by 50%.
A common question is whether fibroids can become cancerous. Cancers arising from myometrium are called leiomyosarcomas. The overall risk of uterine wall tumors being cancerous (malignant) is approximately one in 1,000 in the reproductive years, but is more common in postmenopausal women. A fibroid that grows after menopause may in truth be a leiomyosarcoma, and a hysterectomy to surgically remove the uterus is required.
Now let’s talk about how fibroids can be diagnosed.
Uterine fibroids are often found with a pelvic examination. Other diagnostic procedures may help determine the presence, location, and size of fibroids, and check for other conditions such as ovarian tumors or bowel masses. When a woman has irregular bleeding, a blood test can help determine if the bleeding is because she doesn’t ovulate. An endometrial biopsy may be used to sample a small piece of the endometrium to test for precancerous changes. For some women, diagnostic tests may be helpful in determining the best treatment.
Ultrasound uses the echoes from high frequency sound waves to create a picture of the pelvic organs. Transvaginal ultrasound is typically the first tool used to diagnose uterine fibroids. Since fibroids vary in size and location, both transvaginal and transabdominal ultrasounds may be used to best visualize the fibroids.
Sonohysterography is an ultrasound procedure in which a small amount of fluid is placed in the uterus through a thin plastic tube. Most women experience some mild cramping with insertion of the fluid. The fluid helps visualize an outline of the uterine cavity and improves the ability to identify fibroids which protrude into or distort the space. Sonohysterography can also help determine the best approach for treating the fibroid. The procedure can be performed in your physician’s office.
Hysterosalpingography, or HSG, uses x-ray to produce an image of the inside of your uterus and determine if the fallopian tubes are open. For an HSG, a thin plastic tube is passed through the cervix and an iodine-containing fluid is injected into the uterine cavity and allowed to flow into the fallopian tubes. X-rays are taken during the procedure. Fibroids which protrude into or change the shape of the uterine cavity, or those that block the fallopian tubes can be identified by an HSG.
Magnetic Resonance Imaging (MRI) produces a picture by absorbing energy from specific, high-frequency radio waves that can determine if fibroids are present. An MRI is not routinely needed to diagnose fibroids. However, it may help clarify the diagnosis in some circumstances such as when a woman has deep fibroids that cannot be felt on exam or seen with other procedures or to determine the exact location and size of fibroids in the uterus.
Diagnostic hysteroscopy is useful to determine the presence of submucosal fibroids. With this procedure, a telescope-like instrument called a hysteroscope is inserted through the vagina and cervix into the uterus to look for abnormalities within the uterine cavity. If this procedure is performed in an operating room, a submucosal fibroid may be removed.
Because of the availability of other minimally-invasive procedures, diagnostic laparoscopy is rarely used to diagnose a uterine fibroid. This surgical procedure involves inserting a telescope through the umbilicus and inflating the abdomen with carbon dioxide. The external surface of the reproductive organs can be seen through the laparoscope.
Once a woman has had her uterine fibroids diagnosed, the next step will be to evaluate her treatment options. Fibroids usually don’t require treatment since most women don’t have symptoms. Regular checkups with your physician can determine if you are developing symptoms that would require treatment. This is especially important if you are planning a pregnancy. Women who have symptoms must decide among several treatment options including medical and surgical management.
Medical management for uterine fibroids may help temporarily, but does not improve a woman’s fertility. A group of drugs called GnRH analogs can temporarily reduce the size of fibroids by reducing estrogen production by the ovaries. GnRH analogs can help reduce the size of the fibroids before surgery by up to 50%. Since there is less vaginal bleeding with smaller fibroids, anemia is reduced. In addition, iron supplements are usually recommended. When GnRH analog therapy is discontinued, fibroids will return to their pretreatment size within three to six months.
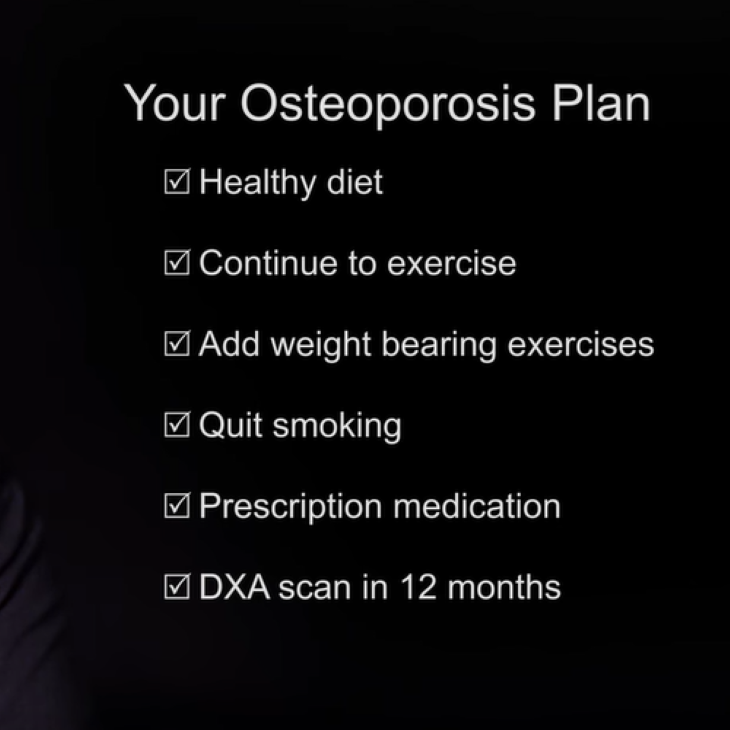
GnRH analogs are given by injection or nasal spray, and produce menopausal-like side effects such as hot flushes, vaginal dryness, mood swings, and sometimes bone loss. These medications cannot be used for extended periods of time unless special precautions are taken to prevent bone loss and menopausal symptoms. These preventive measures may include using low-dose birth control pills, progestins, or doses of estrogens/progestins used in menopausal women.
Hormonal therapies, such as birth control pills and progestins, may be use to help control abnormal uterine bleeding associated with fibroids, but do not affect their size.
Hormonal agents that are made from androgens, or male hormones, can be used to shrink fibroids temporarily. But these drugs are associated with problematic hair growth, voice changes, and other unwanted side effects. One drug that works against progesterone (like RU 486) has been used temporarily in small numbers of women.
Drugs called aromatase inhibitors can be helpful. They prevent the male hormones from converting to estrogens, which decreases symptoms and uterine size in women with fibroids.
Alternative approaches such as herbal and homeopathic therapies have not been shown to improve symptoms caused by fibroids. Although iron therapy may improve anemia, other nutritional modifications are not of proven benefit. None of these approaches can be considered a primary treatment for uterine fibroids at present. Research continues to evaluate other medical therapies.
For women with symptoms, there are a variety of surgery options available to treat uterine fibroids. However, if a woman wants to get pregnant, there are only two surgical options: myomectomy, which is surgical removal of the fibroids, and a procedure called magnetic resonance-guided focused ultrasound surgery (MRgFUS).
There are several ways a myomectomy can be done. In most cases, the size and location of the fibroids will determine the appropriate surgical techniques. Some fibroids may be removed through minimally invasive procedures, such as hysteroscopy, laparoscopy, or robotic procedures. Women with large, multiple fibroids usually require an abdominal myomectomy.
In an abdominal myomectomy, or laparotomy, the surgeon makes an incision in the abdomen and removes the fibroids from the uterus. The hospital stay is usually 24-72 hours with complete recovery in four to six weeks. The two major risks of a myomectomy are excessive blood loss and adhesions (scar tissue) that may impair future fertility. In addition, if surgery involves entering the uterine cavity, there can be scarring in the inside of the uterus. Rarely, a hysterectomy may be required to control hemorrhage. If the myomectomy involves extensive repair to the uterus, a woman may have to have a Cesarean section with a future pregnancy to reduce the risk of uterine rupture during labor.
Hysteroscopic myomectomy may be used to remove submucosal fibroids that are located mainly within the uterine cavity. During this surgery, the physician inserts a telescope through the cervix and fills the uterus with fluid to expand the walls. Surgical instruments are then inserted through a channel in the hysteroscope to remove the submucous fibroids. Generally, women are sent home the same day of surgery and can return to their normal activities within a few days. Serious complications are uncommon but include damage or scarring inside the cavity of the uterus, electrolyte imbalance (changes in the minerals in the blood system), puncturing the uterus, and bleeding. If repairs inside the uterus were extensive, some doctors may place a catheter in your uterus to prevent scarring or prescribe estrogen to accelerate healing of the endometrium. For some women, a hysteroscopic myomectomy may decrease the risk of miscarriage.
A laparoscopic myomectomy can sometimes be used to remove fibroids. During this procedure, the physician inserts a telescope-like instrument into the abdomen through a small incision near the navel. Surgical instruments placed through other small 5-10 mm incisions are used to remove the fibroids. Women can often go home from the hospital the same day or within 24 hours. Recovery time is usually two to seven days. Risks associated with laparoscopic myomectomy include adhesions, trauma to internal organs, and hemorrhage. Women who have this procedure for intramural fibroids may have an increased risk of uterine rupture in future pregnancies. However, there are many studies which have shown no difference in pregnancy outcomes between a myomectomy done through an open incision compared to laparoscopy.
In some cases, robotic technology can be used to remove fibroids. During a robotic myomectomy procedure, the physician places a telescope into the abdomen at or above the navel. As many as five other small incisions are made to insert the instruments used to remove the fibroids. Once the instruments are in place, the physician controls the instruments and performs the surgery from a computer console. Women can usually go home from the hospital the same day, or within 24 hours. Recovery time is usually between a few days and a week. Risks associated with robotic surgery including adhesions and bleeding. Robotic-assisted procedures are helpful for fibroids within the muscle of the uterus and those pushing in on the cavity as the technology makes it easier to close the incisions. Although robotic-assisted myomectomy is relatively new, early studies suggest that outcomes are comparable to abdominal myomectomy and recovery is similar to laparoscopic myomectomy.
The chances of getting pregnant after fibroid surgery are similar to the chances for women in the general population. But it’s important to remember that other factors also influence fertility, such as age, previous pregnancy, ovulatory status, the condition of the fallopian tubes, and the male’s semen quality.
In general, pregnancy rates are between 40%-50% after a myomectomy. Depending on the location of the fibroids, a myomectomy may also decrease the risk of miscarriages. You should talk with your physician to determine your personal clinical profile.
Pregnancy after having a fibroid removed from the uterine muscle may require a scheduled Cesarean section before labor begins. The strong labor contractions needed for a vaginal delivery may result in an increased risk that the uterus will rupture, as well as complications for the baby.
After a myomectomy, there is a chance that fibroids can occur again. This risk of recurrence is 27% over 10 years. Women who have multiple fibroids are more likely to have the fibroids return, while this is less common in women with a single fibroid.
The other option for women with uterine fibroids seeking pregnancy is magnetic resonance (MR)-guided focused ultrasound (MRgFUS). With this procedure, MRI helps locate the fibroid, and high-intensity ultrasound is focused on the fibroids to increase the temperature and break down and destroy the abnormal cells. Other tissues around the fibroid are not affected. There is limited information about long-term outcomes for this relatively new technology.
For women with symptoms from fibroids who do not want to become pregnant, there are a multitude of treatment options.
Another laparoscopic technique called myolysis involves destroying the fibroids through freezing or heat energy using needles or lasers.
Uterine artery embolization is a procedure performed by a radiologist that involves injecting small particles into the uterine blood vessels. These particles clog the small blood vessels that supply the fibroids, blocking the blood supply, and causing the fibroids to degenerate. Women typically have pain for several days after the procedure. The fibroid volume shrinks by 40%-50% and most women have relief of their symptoms.
Approximately half of all hysterectomies are performed to treat uterine fibroids. There are three ways to perform a hysterectomy: abdominally, vaginally and in some cases, laparoscopically. Recovery time ranges from two to six weeks. It’s important to discuss with your physician all aspects of a hysterectomy, including the sexual, psychological, and medical consequences. If your ovaries are removed at the time of the hysterectomy, it’s also important to talk about issues relating to menopause.
In conclusion, uterine fibroids are quite common in women of reproductive age. Symptoms include bleeding, pain, pressure, and infertility. Diagnosis can be made by ultrasound, saline-infused sonography, hysterosalpingogram, hysteroscopy or MRI. Your treatment depends on whether or not you want to become pregnant. For women who want to become pregnant, treatment options include myomectomy and MRgFUS. For those who are finished with their childbearing, hysterectomy, embolization, and ablation can relieve symptoms.
Please see your physician for a customized evaluation, and to decide which treatment options are best for you.
Fertility Preservation
Cancer
Find a Health Professional