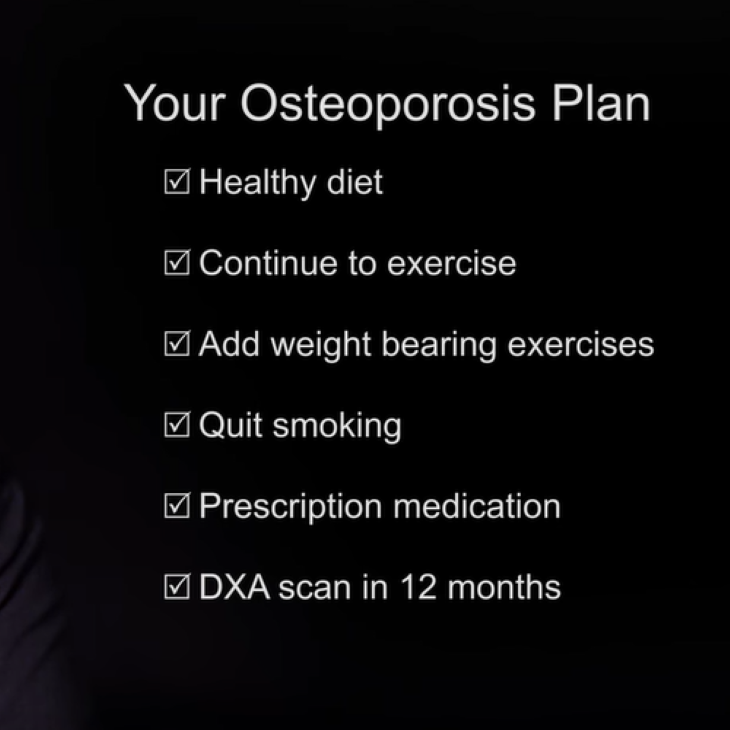
Healthy Sexuality
Sexuality is the experience and/or expression of a person as a sexual being. Sexuality can be different from person to person and can vary over time in an individual.
Transcript
Sexuality is the experience and/or expression of a person as a sexual being. Sexuality can be different from person to person and can vary over time in an individual.
Sex and sexuality are important issues for many people, regardless of their age, sex, or gender. Although many people are embarrassed or afraid to talk about sex or sexuality, it’s important to bring up any concerns with your healthcare provider or sexual counselor.
Let’s begin with some definitions and explanations.
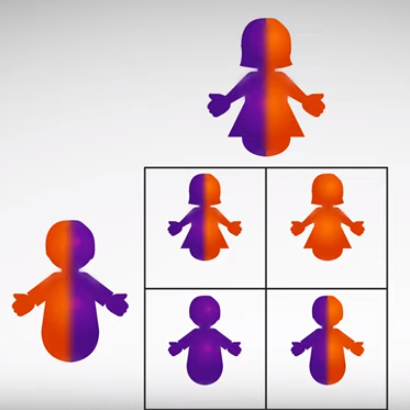
Sexuality is the experience and/or expression of a person as a sexual being. It involves the complex interplay of sex (whether a person is biologically male or female), gender identity (how people identify themselves as male, female or other), gender roles (a person’s expression of social and behavioral norms), and sexual orientation (who a person is sexually attracted to). It’s important to understand that sexuality can be different for each person and may vary over the course of a lifetime.
The World Health Organization has defined sexual health as “…a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction, or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence. For sexual health to be attained and maintained, the sexual rights of all persons must be respected, protected and fulfilled.”
The concept of “sex,” is difficult to define and varies from person to person. There are many ways to express sexuality in all types of relationships, whether between men and women or partners of the same sex. Sex often is considered to be penile-vaginal intercourse between a man and a woman. Other sexual activities, such as oral sex, anal sex, mutual masturbation, etc., can be included where intercourse may not be the goal in the sexual experience. What is most important is that a sexual experience is safe, healthy, and enjoyable.
Sexual health is a vital part of a person’s total well-being. Of course, sex is essential for reproduction, but it can also build intimacy in relationships and be a source of immense pleasure and satisfaction. Sex also has many other positive health benefits, such as reducing stress, improving self-esteem, and cardiovascular health.
A person’s physical sexual response is an important part of his or her sexuality.
Let’s talk about how a woman’s body responds to sexual stimulation.
During sexual arousal, blood flow increases to a woman’s genitals. Her vagina is lubricated by secretions from the walls of the vagina. The vaginal muscles relax, causing the vagina to lengthen and widen. The clitoris grows larger and the labia (the lips of the genitals) become engorged and open, revealing the opening to the vagina. The uterus enlarges and rises upward into the abdomen. Also during this phase, many non-genital changes occur; a woman’s nipples become erect, her blood pressure and heart rate increase, and a “sex flush” from the stomach to breasts and neck develops. During orgasm, also called the climax, there are strong rhythmic contractions of the pelvic floor, the vagina, and uterus. After orgasm, this process may be repeated or the body may return to its unexcited state, called resolution.
There are also physical changes during the sexual response in men. During arousal, a man’s penis becomes filled with blood, causing it to rise and stiffen. The smooth muscles of the scrotum contract, the skin of the scrotum thickens and the testicles are drawn up toward the abdomen. Meanwhile, seminal fluid collects in the prostatic urethra and the bulbourethral glands secrete a few drops of clear liquid at the tip of the penis. While all this is happening, many other changes occur: heart rate and blood pressure increase and some men also develop a sex flush and nipple erection. During orgasm, there are strong, rhythmic contractions of the genital ducts, accessory glands, and penis. Semen is forced through the urethra, called ejaculation. Orgasm and ejaculation often occur close together, but they are actually two separate events. After orgasm, the body returns to its unaroused stated, called resolution.
“Normal” sexual function has been described in many ways by different investigators. Most people think about sexual function as described by Masters and Johnson in the mid-1960s. They described 4 stages, beginning with the “excitement” phase, with psychologic and physical interest and arousal, followed by the “plateau” phase with the peak of sexual arousal, then “orgasm,” which is the climax of the sexual response, and then “resolution,” when the body returns to its unstimulated state.
Since Masters and Johnson, other researchers have modified the original concept with different descriptions of the sexual response. In 1979, desire was added to the sexual reponse model, and then response was changed to only desire, arousal, and orgasm. The thought was that wanting sex or wanting to be sexual is thought to start arousal.
Because a woman’s sexual response is more complex and circuitous than that of a man, and is also affected by many psychosocial factors, other researchers have shown that a women’s response intertwines both her physical and emotional sexual drive. This would explain how women can start, or be receptive to, a sexual encounter. For example, a woman may enter into sexual activity to increase emotional closeness and commitment without having any previous desire or thoughts about sexual activities. As she focuses on the sexual stimulation and sensations, her body begins to respond both physically and psychologically. Continued stimulation produces increased intensive sexual excitement and that produces sexual desire that she may not have had at first.
Sometimes people worry about their sexual health and function.
If you have these concerns, you’re not alone; it’s estimated that 43% of women and 31% of men have experienced some type of sexual concern. Some common concerns are a decrease or loss of interest in sex, the inability to become aroused, problems getting and/or maintaining an erection, a delay or absence of orgasm and pain with sexual activity.
Psychologic factors that may play a role include anxiety, depression, stress, abuse, and poor body image. Memories of a sexual trauma can greatly influence how a person functions sexually. Social and interpersonal factors that can affect sexual function include relationship problems, religious beliefs, cultural beliefs, and one’s upbringing.
When a sexual concern causes distress, it can be classified as a dysfunction.
The second part of this video will cover some types of sexual problems and how they can be treated.
Disorders of sexual dysfunction can be lifelong or they may begin at any stage of life. They can also be situational, meaning they occur only under certain circumstances or with a certain partner, or, they can occur all the time. Sexual disorders affect both men and women and are classified into 4 main categories: sexual desire disorders, sexual arousal disorders, orgasmic disorders, and sexual pain disorders. We’ll discuss each of these briefly.
Sexual aversion disorder is an intense dislike of genital contact with a sexual partner and the person feels disgust and revulsion towards sexual activity. The main feature is avoidance, which is similar to what happens when a person has a phobia or fear.
Hypoactive sexual desire disorder, or HSDD, is having little or no sexual fantasies and desire for sexual activity. This lack of desire is beyond what normally happens in a relationship’s duration and life cycle. The clinical diagnosis of HSDD is subjective and takes into account the person’s age, physical health, and personal life circumstances.
In combined arousal disorder, the woman does not experience physiologic or subjective (mental) arousal. In missed arousal disorder, women have physiologic arousal but not subjective arousal. With genital arousal disorder there is subjective arousal, when the woman is mentally aroused and feels sexual arousal from non-genital stimulation, but she lacks physiologic arousal or vaginal congestion, that is, no pleasurable sexual sensations in her clitoris or vagina.
Male erectile disorder, or ED, is the inability of a man to reach, or maintain an adequate erection until completion of sexual activity. This is a common problem that may be due to many factors, including physical, psychological, medical conditions, or medications.
Men with male orgasmic disorder have a delay in, or absence of, orgasm following a normal sexual excitement phase with sexual activity. In diagnosing this, the clinician takes into account the man’s age, and judges the sexual activity to be adequate in focus, intensity, and duration.
With premature ejaculation, a man ejaculates with minimal sexual stimulation before, on, or shortly after penetration. This can be distressing for both the man and his partner.
Male dyspareunia, or male sexual pain, is very uncommon, and is usually due to a medical condition. There are 4 categories of male sexual pain: 1) ejaculatory pain that occurs occasionally, 2) pain associated with sexual activity as part of a chronic pelvic pain syndrome, 3) painful genital conditions that interfere with sexual activity or are associated with sexual dysfunction, such as chronic testicular pain, and 4) other causes of sexual pain that include conditions of the penis, such as phimosis or a tight frenulum, and other types of sexual pain disorders, for example, anal pain in homosexual men.
Women with female sexual arousal disorder have little or no genital responsiveness to stimulation and they don’t produce adequate lubrication to engage in sexual intercourse. There are several subtypes of female sexual arousal disorders.
Female orgasmic disorder is a delay or lack of orgasm following a normal excitement phase. It’s important to note that many women are able to achieve orgasm with specific forms of stimulation, but not with intercourse, so this is considered within the normal range sexual function.
Female dyspareunia is pain in the vaginal area that occurs before, during, or after sexual intercourse. Pain may occur with entry into the vagina or as deep pain. Both psychological and physical factors can contribute to the condition. Current thinking is that dyspareunia is a pain disorder that interferes with sexuality, as opposed to a sexual disorder characterized by pain. So there may be other possible problems, including vaginal atrophy, vulvodynia, interstitial cystitis, endometriosis, and adhesions. It’s important to note that psychological problems such as sexual abuse can be involved as well. Pain caused by lack of lubrication or by vaginismus is not included in this disorder.
Vaginismus is the involuntary tightening of the outer part of the vaginal muscles that makes vaginal penetration difficult, even when a woman wants sexual penetration. Women with this condition can still achieve orgasm and enjoy sexual activity, just not penetration. Some women with vaginismus can tolerate a pelvic examination, while some women can have intercourse but experience vaginismus during pelvic exams.
Although vaginismus is considered a pain disorder, most women don’t feel pain since penetration is impossible. It’s not clear whether the muscles actually do spasm. Vaginismus is believed to be mostly an anxiety disorder, although physical abnormalities should be checked by a clinician.
If you have a sexual concern, it is important to know that help is available.
Share your concerns with your healthcare provider, who can address the concern or refer you to a specialist trained in the diagnosis and treatment of sexual problems. This specialist may be a physician, psychologist, social worker, or physical therapist. You may also find it helpful to discuss your concerns with your sexual partner.
Because they are complex, sexual concerns are treated in many different ways.
Often, multiple types of treatment may be required and are used together to treat a problem. Education is important in understanding the anatomy and physiology of sex and in having realistic expectations for sex. You might consider reading books and watching videos to learn more about sex.
Making a lifestyle modification can positively impact sex. This can include healthy living, maintaining a normal body weight, exercising, keeping a balanced diet, and minimizing and relieving stress. You can optimize the sexual setting by enhancing communication with your partner, promoting non-sexual intimacy, and finding ways to keep sex special and exciting.
Sexual aids include lubricants, moisturizers, and sexual toys. Lubricants work by reducing friction between tissues. Many different types of lubricants are available, either as water-based, silicone-based, or oil-based products. Water-based lubricants have the advantage of being nonstaining. Silicone-based lubricants stay slippery longer than those that are water-based but may be difficult to wash off since they are water-resistant. A silicone lubricant is safe to use with condoms. Oil-based lubricants (such as petroleum jelly and baby oil) should be avoided, because they are associated with vaginal irritation and may break if used with latex condoms.
Moisturizers also reduce friction between tissues but they are different from lubricants in that they are absorbed into the skin. Moisturizers are a “maintenance therapy” that is applied regularly.
Sexual aids, also known as “sex toys” can be used to enhance sexual pleasure. There are many devices that fall under this category, including vibrators, dilators, and clitoral devices. Vibrators and dildos can be used by men and women to increase sensation to the genitals. Vaginal dilators are used to stretch and relax the vaginal muscles and can be useful in treating women with vaginal stenosis (constriction or tightening) or vaginismus (involuntary tightening of the vaginal muscles). There are many clitoral devices, but only one has FDA-approval for treatment of female sexual dysfunction. The Eros is a small pump-like vacuum that fits over the clitoris and uses suction to increase blood flow into the clitoris so that it swells, enhancing sensitivity.
Sex therapy and counseling may involve individual and couples sessions, cognitive behavioral therapy, and sensate focus, which are types of specific sexual exercises. Sex therapists and counselors are mental health providers who have specialized training in working with people with sexual concerns. Cognitive behavioral therapy is a type of psychotherapy that focuses on how one’s thinking influences feelings and behavior. Sensate focus exercises are structured “touching” activities that are designed to help couples increase their comfort with physical intimacy and familiarize themselves with each other’s (and their own) body.
Physical therapy can include Kegel exercises, biofeedback therapy, and pelvic floor muscle rehabilitation. Kegel exercises involve contracting and relaxing the muscles of the pelvic floor to increase strength and tone. Biofeedback therapy involves the placement of biofeedback sensors that allow an individual to “see” their actions. In addition to improving sexual function, pelvic floor muscle rehabilitation can improve pelvic pain and urinary incontinence.
Medical therapy may include hormone therapy, antidepressants, phosphodiesterase inhibitors, which are drugs often used for erectile dysfunction, and other medications. For women estrogen can be given systemically or vaginally, depending on the presence of other symptoms. Systemic estrogen therapy can be useful for women experiencing multiple symptoms of estrogen deficiency, such as hot flushes, vaginal dryness, and night sweats. For women who have vaginal symptoms only, vaginal estrogen can be prescribed. Vaginal estrogen is a moisturizer that comes in a variety of forms, including a cream, tablet, or a ring. Although testosterone is not FDA-approved for treatment of low desire in women, there is some evidence that it may improve sexual experiences in postmenopausal women. This use is controversial, especially in premenopausal women. Another androgen, dehydroepiandrosterone (DHEA), has been proposed to improve libido in women, however more studies are needed to confirm its efficacy and safety.
For men with low testosterone levels, there is some evidence that testosterone therapy may improve sexual function.
A group of antidepressant drugs called selective serotonin reuptake inhibitors, or SSRIs, often reduce sexual desire and response. However, some other antidepressants have been shown to improve sexual desire. In a small study of nondepressed women and men with desire and arousal difficulties, buproprion improved sexual functioning compared with placebo.. Larger studies are needed to confirm these findings. Another antidepressant, flibanserin, was recently rejected for approval by the FDA because it produced only small improvements in response rates compared with placebo and was associated with several side effects.
Phosphodiesterase inhibitors such as sildenafil, vardenafil, and tadalafil, are approved for treatment of erectile dysfunction in men. Women who were given sildenafil in studies also had increased blood flow to the genitals, this did not result in any real increase in desire or arousal compared with placebo.
There are many other herbs, supplements, and other “natural” products that are advertised to improve sexual performance or satisfaction. These products are not regulated by the FDA, so their safety and effectiveness is largely unknown.
Surgical therapy includes penile implants and vestibulectomy. Penile implants are devices inserted inside the penis that allow men with erectile dysfunction to get an erection. During a vestibulectomy, pain fibers are removed from the vaginal vestibule for the treatment of vulvodynia.
Sex is an important part of your life and sexual concerns should be taken seriously.
When a sexual problem causes you distress, don’t be afraid to talk with a healthcare professional. Although sexual problems can be complex, there are a variety of treatments that can be very effective. With the appropriate diagnosis and treatment, everyone can achieve the healthy and satisfying sex life that they deserve.
Find a Health Professional