Revised 2016
INTRODUCTION
Hirsutism is the excessive growth of facial or body hair on women. Hirsutism can be seen as coarse, dark hair that may appear on the face, chest, abdomen, back, upper arms, or upper legs. Hirsutism is a symptom of medical disorders associated with the hormones called androgens. Polycystic ovary syndrome (PCOS), in which the ovaries produce excessive amounts of androgens, is the most common cause of hirsutism and may affect up to 10% of women. Hirsutism is very common and often improves with medical management. Prompt medical attention is important because delaying treatment makes the treatment more difficult and may have long-term health consequences.
OVERVIEW OF NORMAL HAIR GROWTH
Understanding the process of normal hair growth will help you understand hirsutism. Each hair grows from a follicle deep in your skin. As long as these follicles are not completely destroyed, hair will continue to grow even if the shaft, which is the part of the hair that appears above the skin, is plucked or removed. Hair follicles cover every surface of your body except the soles of your feet and the palms of your hands. Of the approximately 50 million hair follicles covering your body, one fifth are located on your scalp. The number of hair follicles you have does not increase after birth but slowly begins to decrease at around age 40.
Hair density varies by ethnic origin. Men and women of the same ethnic group have similar numbers of hair follicles and similar hair patterns. People of Mediterranean descent, for example, generally have much more hair than Asians and American Indians. Excessive hair that is due to genetic and ethnic variation rather than hormonal causes is typically located on the arms, hands, legs, and feet, whereas hirsutism typically affects the face, abdomen, chest, inner thighs, and back.
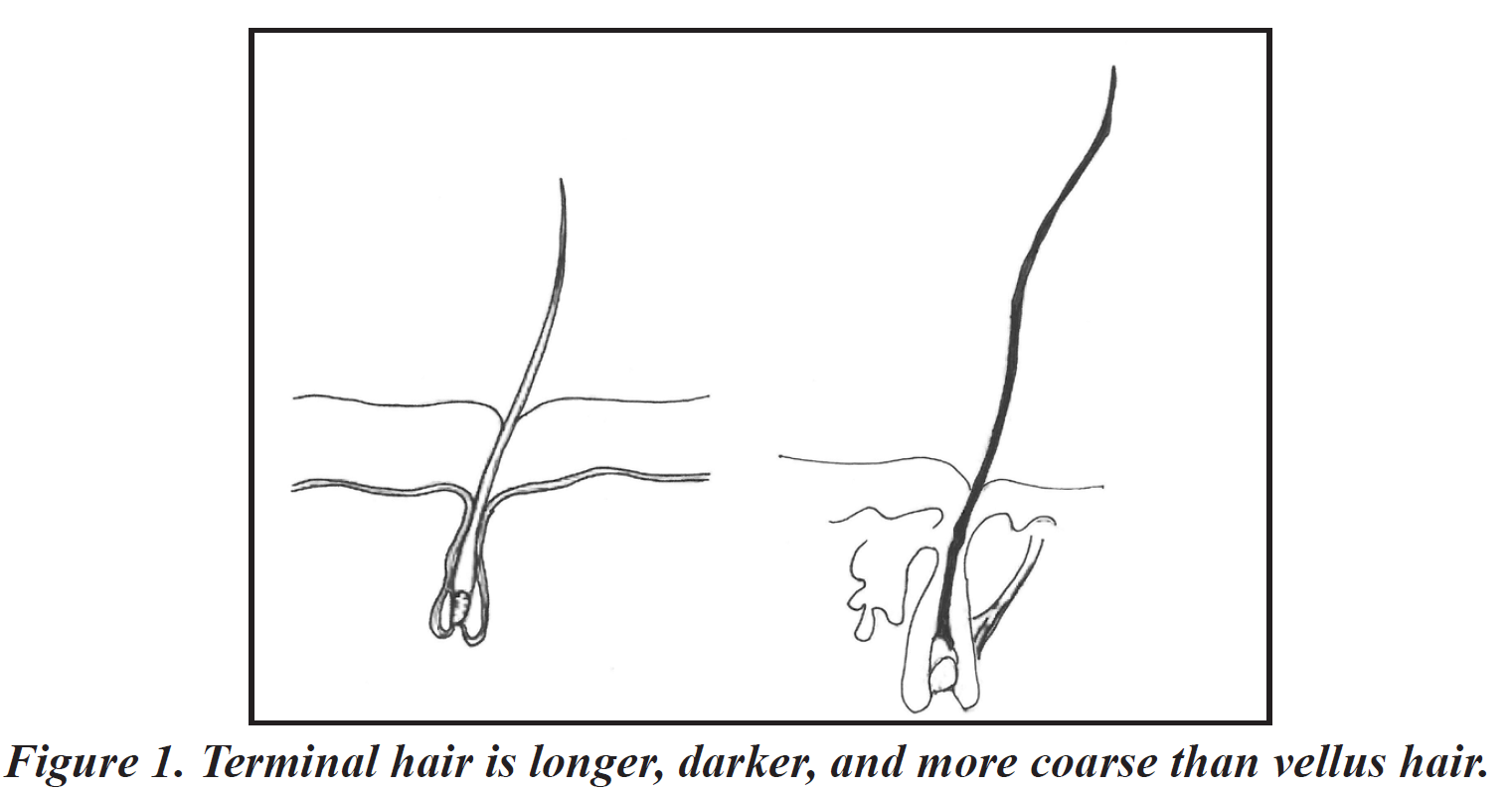
Adults have two types of hair, vellus and terminal (Figure 1). Vellus hair is soft, fine, generally colorless, and usually short. Terminal hair is long, coarse, dark, and sometimes curly. In most women, vellus hair covers the face, chest, and back and gives the impression of “hairless” skin. In most men, terminal hair covers the face and body. Terminal hair grows on the scalp, pubic, and armpit areas in both men and women. A mixture of vellus and terminal hair covers the lower arms and legs in both men and women. If excessive hair growth is present only on your lower legs and forearms, it is not considered hirsutism and will not respond to hormonal therapy.
Hair growth occurs in cycles. While some hair follicles grow, others rest, and still others are shed. Hormonal changes, such as those associated with oral contraceptives (birth control pills) or pregnancy, may synchronize hair growth and make it appear to grow and shed more than usual. However, hair growth patterns usually return to normal within 6 to 12 months.
Figure 1
EFFECTS OF ANDROGENS ON HAIR GROWTH
 Excess facial and body hair is usually the result of excess androgens in your body. Androgens are present in both men and women, but men have much higher levels of biologically active androgens. In men, androgens are produced primarily by the testes and the adrenal glands. In women, androgens are produced by the ovaries and the adrenal glands. To some degree, estrogen reduces the effect of androgens in women.
Excess facial and body hair is usually the result of excess androgens in your body. Androgens are present in both men and women, but men have much higher levels of biologically active androgens. In men, androgens are produced primarily by the testes and the adrenal glands. In women, androgens are produced by the ovaries and the adrenal glands. To some degree, estrogen reduces the effect of androgens in women.
If your hair follicles are hormone-sensitive, androgens may cause some vellus hairs to change to terminal hairs and cause the terminal hairs to Figure 1. Terminal hair is longer, darker, and more coarse than vellus hair, grow faster and thicker (Table 1). Once a vellus hair has changed to a terminal hair, usually it does not change back. Androgens increase sebum production, which results in oily skin and acne. Excess androgens can cause irregular or absent ovulation and menstruation. Extremely high androgen levels, such as when a tumor is present, may cause male-like balding, deepening of the voice, increased muscle mass, enlargement of the clitoris, and decreased breast size. These effects of excess androgens are called virilization, occur rarely, and typically are not seen with PCOS.
Table 1. Androgen-sensitive sites of hair growth
| MORE COMMON | LESS COMMON |
| Upper lip | Chest and sternum |
| Beard area | Upper abdomen |
| Breasts | Upper back |
| Lower abdomen | |
| Inner thighs | |
| Lower back |
DIAGNOSING HIRSUTISM
 Physicians trained to treat hirsutism and related problems generally include reproductive and medical endocrinologists. Some gynecologists, dermatologists, and general practitioners also have acquired the necessary expertise. During your initial medical consultation, your physician will try first to make a distinction between terminal hairs growing in a male pattern indicating hirsutism and hair growth due to genetic or ethnic predisposition. If you are diagnosed with hirsutism, your physician may perform blood tests, ultrasound, special x-rays, and hormone tests to evaluate the function of your ovaries and adrenal glands. After identifying the causes of hirsutism, your physician can recommend appropriate treatment. Any unwanted hair remaining after treatment may be removed by a variety of cosmetic treatments, including laser and electrolysis.
Physicians trained to treat hirsutism and related problems generally include reproductive and medical endocrinologists. Some gynecologists, dermatologists, and general practitioners also have acquired the necessary expertise. During your initial medical consultation, your physician will try first to make a distinction between terminal hairs growing in a male pattern indicating hirsutism and hair growth due to genetic or ethnic predisposition. If you are diagnosed with hirsutism, your physician may perform blood tests, ultrasound, special x-rays, and hormone tests to evaluate the function of your ovaries and adrenal glands. After identifying the causes of hirsutism, your physician can recommend appropriate treatment. Any unwanted hair remaining after treatment may be removed by a variety of cosmetic treatments, including laser and electrolysis.
CAUSES OF HIRSUTISM
Hirsutism has several causes, which are summarized in Table 2 and described below:
Table 2. Causes of hirsutism
|
Polycystic Ovary Syndrome
Polycystic ovary syndrome is a common hormonal disorder that affects 5% –10% of women. Because of the variable nature of PCOS, its diagnosis is based upon the combination of clinical, ultrasound, and laboratory features.
Polycystic ovary syndrome is a condition associated with hormonal imbalances that cause the ovaries to overproduce androgens. It is a common cause of hirsutism. In women with PCOS, multiple small follicles develop in the ovaries that appear as cysts, hence the term “polycystic.” These small cysts are actually immature ovarian follicles that failed to mature and ovulate. PCOS is discussed in greater detail later in this booklet.
 Unexplained Hirsutism
Unexplained Hirsutism
For unknown reasons, some women have hair follicles that are abnormally sensitive to androgens. Androgen levels are normal and menstrual periods occur regularly in these patients. This tendency to develop hirsutism is clearly genetic, but the exact abnormality is not known.
Non-classical Adrenal Hyperplasia
The most common abnormality of the adrenal glands that can result in hirsutism is an inherited disorder called non-classical adrenal hyperplasia (NCAH), which causes the adrenal glands to overproduce androgens. Like PCOS, NCAH is associated with irregular menstrual cycles. NCAH is a genetic disorder most commonly seen in certain ethnic groups, including Ashkenazi Jews, Eskimos, and French-Canadians. Elevation of the hormone 17 alpha-hydroxyprogesterone is characteristic of NCAH.
HAIR-AN Syndrome (Hyperandrogenism, Insulin Resistance, Acanthosis Nigricans)
Some women are born with insulin resistance, a defect in the ability of insulin to control blood sugar levels. To compensate, the pancreas produces more insulin. Excessively high levels of insulin stimulate the ovaries to dramatically overproduce androgens, leading to hirsutism, acne, and irregular ovulation. Insulin resistance may lead to diabetes mellitus, high blood pressure, heart disease, and excessive growth and darkening of the skin (acanthosis nigricans), which generally occurs around the neck and crease areas of the skin. The majority of these severe cases are due to genetic abnormalities. HAIR-AN syndrome is not to be confused with the milder insulin resistance seen in PCOS and other forms of hyperandrogenism. These women, however, do have polycystic ovaries.
Cushing Syndrome
 Cushing syndrome refers to overproduction of cortisol by the adrenal glands. Although hirsutism may be seen in Cushing syndrome patients, it is not the primary feature of the disorder. Women with Cushing syndrome often are obese with a flushed and rounded face, muscle weakness, diabetes, and irregular menses. Features of Cushing syndrome also may be found in women who are taking chronic steroid therapy. Cushing syndrome is a serious but rare disease. The hirsutism commonly arises late compared with other signs and symptoms of Cushing syndrome.
Cushing syndrome refers to overproduction of cortisol by the adrenal glands. Although hirsutism may be seen in Cushing syndrome patients, it is not the primary feature of the disorder. Women with Cushing syndrome often are obese with a flushed and rounded face, muscle weakness, diabetes, and irregular menses. Features of Cushing syndrome also may be found in women who are taking chronic steroid therapy. Cushing syndrome is a serious but rare disease. The hirsutism commonly arises late compared with other signs and symptoms of Cushing syndrome.
Ovarian or Adrenal Tumors
On rare occasions, an androgen-producing tumor may develop in the ovaries or adrenal glands. This tumor may produce extremely high androgen levels. Symptoms, such as hirsutism, usually appear suddenly and progress quickly. Very high androgen levels may cause male-like balding, deepening of the voice, and increased muscle mass. Fortunately, most of these tumors are not cancerous.
Menopause
Around the time of menopause, the ovaries stop producing estrogen but continue to produce androgens. The decreased levels of estrogen may allow the androgens to have a greater impact, leading to an increase in the number of dark terminal hairs, especially on the face. For this reason, many menopausal women complain of new facial hair (moustache and whiskers) and mild balding.
Medication Side Effects
Drugs with characteristics of androgens may cause hirsutism. Anabolic steroids, used for increasing the muscle mass of chronically ill and debilitated people and by some bodybuilders, are chemically related to androgens. Other medications associated with increased hair growth include danazol, phenytoin, minoxidil, and diazoxide. Patients on these medications develop acne more frequently than hirsutism. “Natural” supplements such as dehydroepiandrosterone (DHEA) and androstenedione may cause hirsutism.
HOW IS HIRSUTISM TREATED?
Medical Therapy
There are a variety of specific medical and surgical treatments that your physician may recommend based on your diagnosis and severity of hirsutism (Table 3). Most medications used to treat hirsutism are approved by the US Food and Drug Administration (FDA) but not for this specific indication. Nevertheless, research has documented their effectiveness.
Table 3. Treatment of hirsutism
| MEDICATIONS | COSMETIC TREATMENTS |
| Birth control pills | Shaving |
| Androgen receptor blockers | Eflornithine cream |
| Spironolactone | Waxing |
| Flutamide | Bleaching |
| Glucocorticosteroids | Plucking |
| Dexamethasone | Depilatory agents |
| Prednisone | Electrolysis |
| Methylprednisolone | Laser |
| Enzyme inhibitors | |
| Finasteride | |
| GnRH analogs |
Birth Control Pills (Oral Contraceptives)
Birth control pills are the most commonly suggested hormonal treatment for hirsutism. They prevent ovulation and decrease the production of androgens by the ovaries. Estrogen in the pills causes the liver to produce and release more of a protein called sex hormone-binding globulin (SHBG) that binds to androgens and reduces their action. In addition to slowing excessive hair growth, the pills provide the added advantages of regulating the menstrual cycle and protecting against unwanted pregnancies.
Anti-androgenic Medications
Spironolactone, a diuretic or “water pill,” often is prescribed in combination with birth control pills. It has been found to directly block the effects of androgens in hair follicles and has been used to treat hirsutism. Side effects may include dry skin, heartburn, headaches, irregular vaginal bleeding, and fatigue. More than two thirds of the women on highdose spironolactone will have a significant decrease in hirsutism. Other anti-androgenic medications include flutamide, which blocks androgen receptors, and finasteride, which blocks the conversion of testosterone to more active androgens. Side effects can include rare but harmful effects to the liver. These medications are not FDA-approved for the treatment of hirsutism in women but are used commonly and have been studied for that purpose.
Steroid Medications
Low doses of steroids may be prescribed for overactive adrenal glands. Some women taking them experience dizziness during the day, experience mood changes, or have difficulty falling asleep, although these complaints generally improve after the first few days. These drugs may have serious side effects, including weight gain, thinning of the skin and bones, and decreased defense against infection. However, these side effects seldom are seen at the low doses used for treating hirsutism.
GnRH Analogs
Severe forms of hyperandrogenism may be treated by a gonadotropinreleasing hormone (GnRH) analog. These medications treat hirsutism by suppressing ovarian androgens to very low levels. They also suppress estrogen and may cause menopausal-like symptoms. GnRH antagonists are a type of GnRH analog that also are effective and may be approved for use for this purpose in the future. Use of these medications requires close supervision by your physician. An estrogen and/or a progestin often are administered with the GnRH analog to prevent bone loss.
Cosmetic Therapy
Cosmetic removal of hair in women with hormonally associated hirsutism always should be accompanied by medical therapy in order to be successful.
Temporary Hair Removal
For temporary treatment of mild hirsutism, many women pluck unwanted hairs. However, plucking tears the hair from its living follicle and can irritate sensitive skin. If the hair follicle or shaft becomes infected, the hair may curl into the skin and cause pimples or acne. Waxing carries the same risks of irritation and infection, especially in androgen-sensitive areas. Depilatories are chemicals that dissolve the hair shafts and may cause irritation to sensitive facial skin. Bleaching can be used in small areas of the body, particularly the upper lip, to make excessive hair less noticeable, but excessive bleaching may lead to irritation and skin damage.
Although not satisfying to many women, shaving is probably the simplest and safest way to temporarily remove hair. Because of the continued growth of the hair, shaving is required frequently and may result in irritating stubble, but an electric razor may produce less skin irritation than a blade. Shaving seldom has medical side effects.
A facial cream containing eflornithine hydrochloride may be used in combination with the previously mentioned cosmetic therapies to slow the growth of excessive facial hair. Some women have worsening of acne with eflornithine use. Its safety in pregnancy or effectiveness on other body parts has not been established.
Permanent Hair Removal
There are two types of permanent hair removal: electrolysis and laser treatment. During electrolysis, a very fine needle is inserted into the hair follicle. A mild electric current is sent through the needle to permanently destroy the hair follicle’s ability to produce hair. Since follicles are treated one at a time, it is somewhat impractical to use electrolysis to treat very large areas of the body.
Laser treatments may be used on large areas of the body, although their long-term effectiveness is not as well documented as electrolysis. During laser hair treatment, a beam of light is passed through the skin to the hair follicle to destroy it. People with light skin and dark hair usually achieve the best results with laser hair removal.
Both methods of hair reduction are moderately painful, depending on the area of skin being treated, and multiple treatments usually are required. Nevertheless, electrolysis and laser are very effective ways to remove unwanted hair. However, they may not reduce all hair growth and may not always be permanent. Without concurrent medical treatment, new hair will grow. It is best to delay laser or electrolysis treatment for at least 6 months after beginning medical treatment so that the growth of new terminal hairs will be reduced. Physicians often can refer patients to a reputable electrologist or laser specialist. Home electrolysis kits rarely work because the follicle is so deep within the skin that it is difficult to treat.
WHAT TO EXPECT FROM TREATMENT OF HIRSUTISM
Hormone treatment generally prevents new terminal hairs from developing and may slow the growth rate of existing hairs. Generally about 6 months of hormone therapy is required before the rate of hair growth decreases significantly. Once a hormone treatment has proven to be effective, it may be continued indefinitely. Electrolysis or laser can remove any hair remaining after hormone therapy. Because it usually is not possible to cure the hormonal problem that causes hirsutism, ongoing medical treatment is required to manage it. Hirsutism will frequently return if medical treatment is stopped. Sometimes a combination of treatment methods is needed for best results.
POLYCYSTIC OVARY SYNDROME
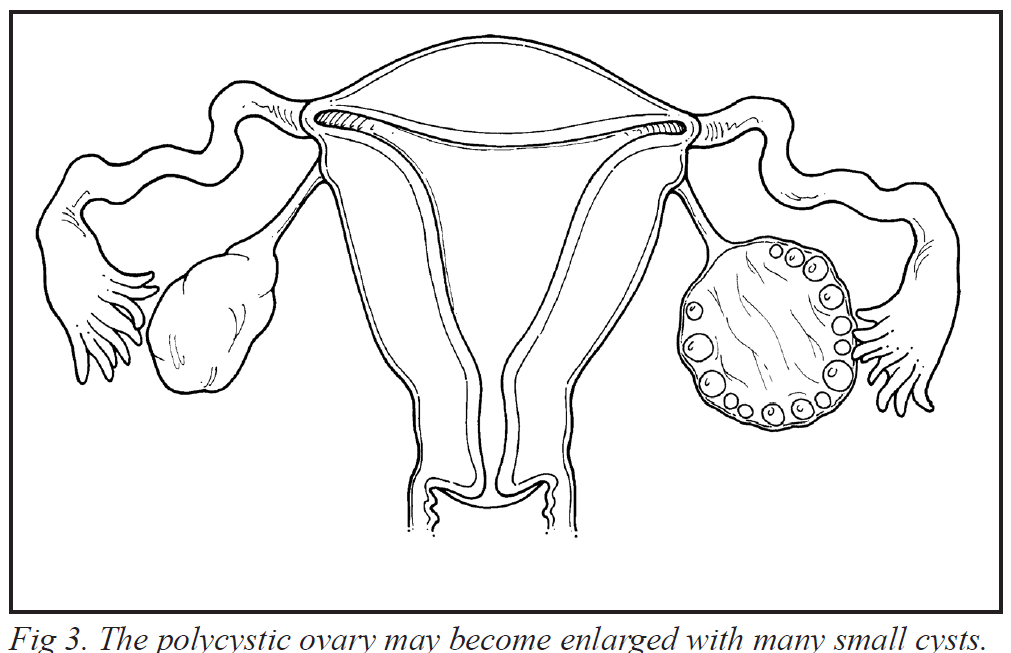
The most common cause of hirsutism is PCOS. PCOS is a term used to describe a common hormonal disorder that causes the ovaries to produce excessive amounts of androgens. The ovaries may become enlarged with many small follicles that appear like cysts (fluid-filled sacs) (Figures 2 and 3). These follicles are different from hair follicles as these ovarian follicles contain eggs. Symptoms of PCOS include hirsutism; acne; irregular, absent, or heavy menstrual periods; lack of ovulation; and infertility. More than 50% of PCOS patients also are overweight or obese, but that is not part of the definition, and some women are of normal weight. Despite persistent questions surrounding the cause of PCOS, many advances have been made in treating this disorder.
Figure 2
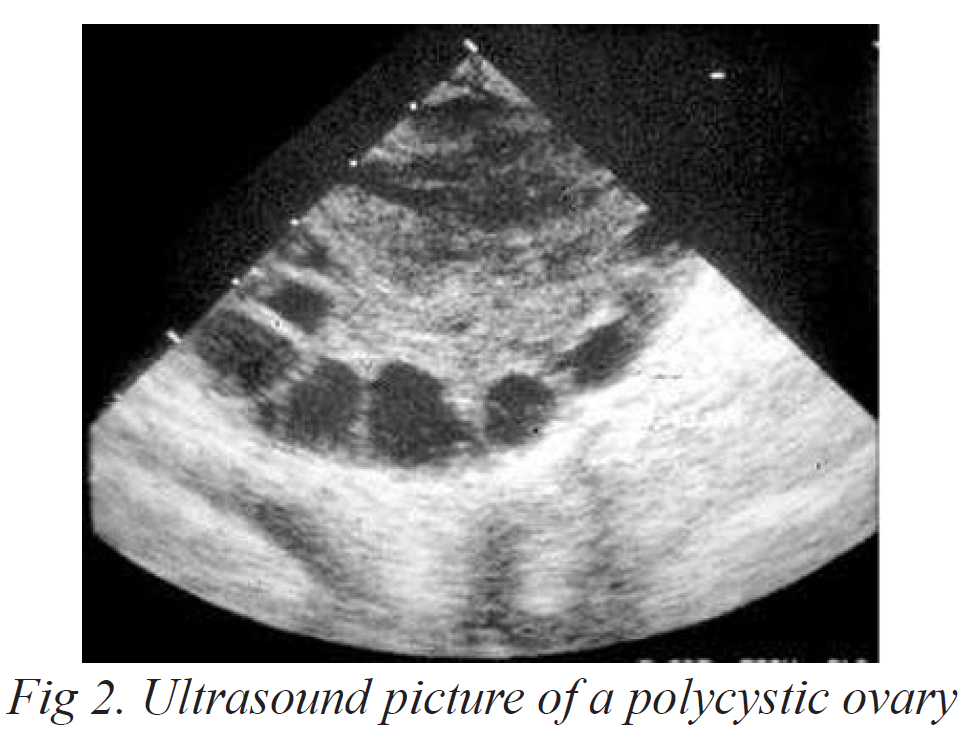
Figure 3
Normal Menstrual Function
In order to understand PCOS, it is important to understand how hormones control normal ovarian function. The pituitary gland, located at the base of the brain, controls egg and hormone production by releasing two hormones, follicle-stimulating hormone (FSH) and luteinizing hormone (LH). As the menstrual period begins, FSH stimulates a follicle in the ovary to begin growing. The follicle produces the hormone estrogen and contains a maturing egg. Luteinizing hormone stimulates the cells surrounding the follicle to produce significant amounts of androgens. The enlarging ovarian follicle (containing an egg) appears as a small cyst on the surface of the ovary that can be detected by ultrasound. Fig 2. Ultrasound picture of a polycystic ovary Fig 3. The polycystic ovary may become enlarged with many small cysts.
About 2 weeks before the onset of the next menstrual period, the follicle ruptures and releases (ovulates) the egg. The cells lining the collapsed follicle begin to produce the hormone progesterone. The follicle is now known as a corpus luteum and secretes estrogen and large quantities of progesterone throughout the second half of the menstrual cycle, which is called the luteal phase.
After ovulation, the egg is picked up by the fallopian tube. If the egg is fertilized, it remains in the fallopian tube for 3 or 4 days and then enters the uterus. The estrogen and progesterone secreted during the luteal phase have prepared the uterus to receive a fertilized egg (embryo). If the egg is not fertilized or the embryo fails to implant in the uterus, the secretion of estrogen and progesterone declines about 2 weeks after ovulation, and the lining of the uterus is shed. This results in menstruation, and the cycle begins again.
Abnormal Menstrual Function
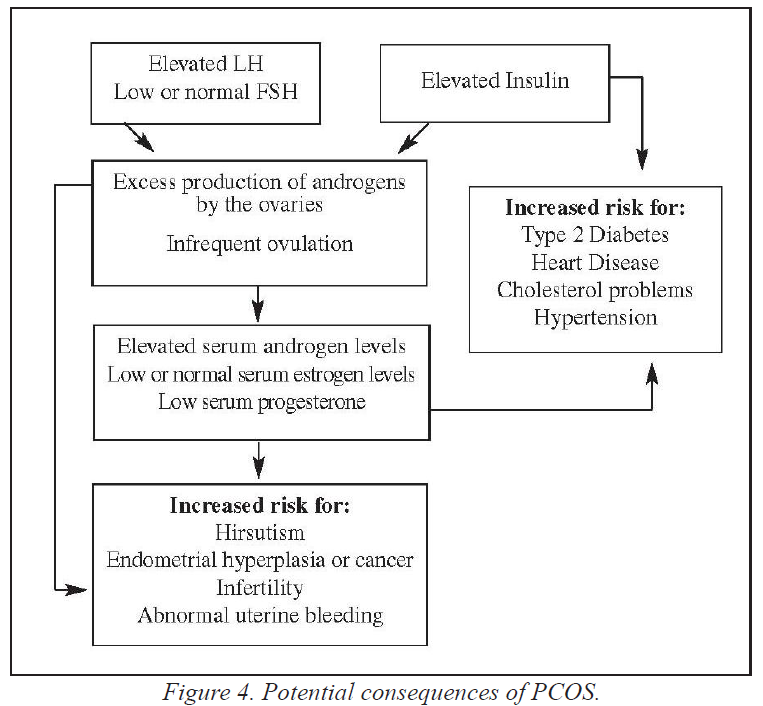
The ovulatory cycle is easily affected by hormonal abnormalities. Overproduction or underproduction of certain hormones can affect many different body symptoms. Excess LH or insulin may cause the ovaries to overproduce androgens.
Insufficient FSH may impair ovarian follicle development and prevent ovulation, resulting in infertility. Eventually, the multiple small cysts formed in the ovary from follicles that failed to mature and ovulate result in the PCOS appearance on ultrasound. Not all women with PCOS have ovaries with this appearance.
Lack of ovulation in PCOS results in continuous high levels of estrogen and insufficient progesterone. Without progesterone, ongoing estrogen exposure may cause the endometrium to become excessively thickened. This can lead to heavy and/or irregular bleeding (abnormal or anovulatory uterine bleeding). Over many years, endometrial cancer may result due to continuous stimulation by high levels of estrogen with low levels of progesterone.
DIAGNOSING PCOS
You should describe all of your symptoms to your physician as specifically as possible. PCOS may be suspected by your medical history and physical examination. To confirm the diagnosis and exclude certain other conditions, your physician may measure your blood hormone levels. If you report irregular menstrual bleeding patterns, your doctor may perform an endometrial biopsy to make sure no precancerous cells are present in your uterus. Because PCOS is not fully understood, it often is difficult to determine why it occurs.
Early Diagnosis
If you have had menstrual irregularity and/or progressive hirsutism since puberty, you should be evaluated for PCOS. If you are diagnosed with PCOS and you have female children, you should watch them for symptoms and inform them that they are at risk, since there is a genetic tendency to inherit the syndrome. Early treatment of PCOS may decrease the development of acne and hirsutism.
Long-term Considerations
Women with PCOS are at risk for metabolic syndrome. Metabolic syndrome is when women develop multiple risk factors for heart disease. and other health problems. Metabolic syndrome is common in women with PCOS, even adolescents. Women may have prediabetes, particularly those with insulin resistance, and may be at an increased risk for diabetes, heart disease, cholesterol abnormalities, and endometrial cancer (Figure 4). If you are diagnosed with PCOS, you and your physician should discuss the long-term health consequences and any additional testing that should be done.
PCOS TREATMENT
If you are diagnosed with PCOS, treatment will depend upon your goals. Some patients may be concerned primarily with fertility, while others are more concerned about menstrual cycle regulation, hirsutism, or acne. Regardless of your primary goal, PCOS should be treated because of the long-term health risks such as heart disease and endometrial cancer.
Weight Loss
Obesity commonly is associated with PCOS. Fatty tissues produce excess estrogen, which in turn contributes to insufficient FSH secretion by the pituitary gland. Insufficient FSH prevents ovulation and may worsen PCOS. In addition, obesity is associated with the development or worsening of insulin resistance, which may further increase androgen production by the ovaries.
Figure 4
Weight loss improves the hormonal condition of many PCOS patients. If you are overweight, ask your physician to recommend a weight-control plan or clinic. Area hospitals and support groups also are helpful. Although tempting, fad diets and diet pills usually are not effective and in many cases cause additional health problems.
Increasing physical activity is an important step in any weight reduction program. Start slowly with an aerobic activity such as walking or swimming. Increase speed and distance gradually. Regular activity improves state of mind as well as aiding in weight reduction. Recommendations include three to four exercise periods each week with at least 30 minutes of aerobic exercise. Extreme cases of obesity, unresponsive to medical management and behavioral modification, may be treated with bariatric surgery. Surgical risks have decreased over time and many procedures are performed in a minimally invasive way. Figure 4. Potential consequences of PCOS.
PCOS Treatment for Women Who Do Not Wish To Conceive
Hormonal treatment frequently is successful in temporarily correcting the problems associated with PCOS. If treatment is stopped, however, symptoms usually reappear.
If you are not trying to conceive, birth control pills may be your best hormonal treatment. Birth control pills decrease ovarian hormone production and help reverse the effects of excessive androgen levels. However, birth control pills are not recommended if you smoke and are over age 35. If you also have hirsutism, your physician may prescribe spironolactone, alone or combined with birth control pills. Rarely, GnRH analogs may be used to decrease ovarian androgen production. If you are not concerned with fertility or contraception, and hirsutism is not a problem, your doctor may prescribe taking progesterone at regular intervals to regulate your menstrual bleeding and prevent the endometrial problems associated with excessive estrogen exposure.
PCOS Treatment for Women Who Wish to Conceive
If fertility is your immediate goal, ovulation may be induced with clomiphene citrate. Clomiphene is simple to use, is relatively inexpensive, and works well to induce ovulation in many patients. Clomiphene causes the pituitary gland to increase FSH secretion which helps stimulate your eggs to mature, sometimes leading to ovulation. Sometimes increasing the dosage or the length of treatment is necessary. Approximately 10% of pregnancies with clomiphene are twins; triplets or more are rare. Your physician also may recommend a steroid drug designed to suppress the adrenal gland to supplement clomiphene therapy. If consistent ovulation is not noted with clomiphene, the use of another oral medication, letrozole, may be considered. Recent studies suggest that pregnancy rates achieved with letrozole use are similar to clomiphene citrate. Letrozole is not approved by the FDA for induction of ovulation. Neither letrozole nor clomiphene citrate should be given to women who are already pregnant because it might lead to abnormalities of the reproductive system in any resulting children.
If clomiphene or letrozole do not induce ovulation, or you do not get pregnant within six ovulatory cycles, your physician may prescribe gonadotropins. There are many types of gonadotropins used alone or in combination for ovulation induction. They include human menopausal gonadotropin (hMG), purified human follicle-stimulating hormone (hFSH), recombinant follicle-stimulating hormone (rFSH), and human chorionic gonadotropin (hCG). Gonadotropins are more expensive and have a higher incidence of side effects such as hyperstimulation (excessive swelling) of the ovaries and a higher rate of multiple pregnancy such as twins or triplets.
Your needs and response to therapy will determine the appropriate medication for ovulation induction. For additional information, consult the ASRM patient information booklet titled Medications for Inducing Ovulation.
In very rare cases, ovulation is not achieved with either clomiphene or gonadotropins, and ovarian surgery may be tried to stimulate ovulation. Surgical procedures such as ovarian drilling may be performed through laparoscopy. Although these procedures have helped some patients to ovulate, they also may have adverse effects on future fertility by causing adhesions (scar tissue) and are generally treatments of last resort.
Metabolic Changes
PCOS increases the risk of metabolic disorders. If you have been diagnosed with PCOS, it is important to be screened for risks associated with metabolic disorders such as heart disease, diabetes and pre-diabetes, elevated cholesterol levels, and high blood pressure. It is important to have these risk factors assessed and treated.
PSYCHOLOGICAL ASPECTS OF HIRSUTISM AND PCOS
Dealing with hirsutism and PCOS can be emotionally difficult. You may feel unfeminine, uncomfortable, or self-conscious about your excessive hair growth or weight, as well as worried about your ability to have children. Even though you may be embarrassed to share these feelings with other people, it is very important to talk with your physician as soon as possible to explore the medical and cosmetic treatments available to treat these disorders. It also is important for you to realize that these are very common problems experienced by many women.
SUMMARY
Hirsutism is a common disorder that usually can be treated successfully with medication. Following medical treatment, electrolysis or laser treatment can be used to permanently reduce or remove any remaining unwanted hair. If other female family members have experienced excessive hair growth, you should watch for early signs of hirsutism in yourself and your children, especially during adolescence. Hirsutism is frequently a result of PCOS. Both hirsutism and PCOS are easier to treat when diagnosed at a young age.
PCOS can cause hirsutism, acne, irregular or heavy menstrual periods, lack of ovulation, and infertility. It also is associated with an increased risk of diabetes, uterine cancer, high cholesterol, and heart disease. Despite questions surrounding the causes of PCOS, advances have been made in both understanding and treating the condition. If you are diagnosed with hirsutism or PCOS, your goals and concerns can be addressed in a relatively short period of time, and treatment often is successful.
Glossary
Adrenal glands. Glands located on top of the kidneys, in the area of the back near the waistline, that produce hormones (cortisol, adrenaline, androgens, and other hormones) that help the body withstand stress and regulate metabolism. Altered function of these glands can disrupt menstruation.
Adrenal hyperplasia. An abnormal or unusual increase in the production of androgens by the adrenal glands. This disorder is the result of a genetic problem.
Androgens. Hormones produced by the testes, ovaries, and adrenal glands responsible for encouraging masculine characteristics. Often referred to as “male” hormones. Androgens are produced in males and females, but males have much higher levels.
Androstenedione. An androgenic hormone naturally made by the ovaries, testes, and adrenal glands. The body turns it into testosterone. Androstenedione sold as a “natural” supplement is made from plant chemicals and is not regulated by the FDA. It often is marketed as an enhancer of athletic performance and muscle strength, but its safety and effectiveness are controversial.
Birth control pills. Also known as oral contraceptives. They contain a mixture of synthetic estrogens and progesterone. Proper usage suppresses ovulation and decreases the ovarian secretion of hormones, including androgens.
Clomiphene citrate. An anti-estrogen drug used to induce ovulation.
Corpus luteum. Literally, a “yellow body.” A mass of yellow tissue formed in the ovary from a mature follicle that has collapsed after releasing its egg at ovulation. The corpus luteum secretes estrogen and large quantities of progesterone, a hormone that prepares the lining of the uterus (endometrium) to support a pregnancy.
Cortisol. A hormone produced by the adrenal glands, which are located on top of the kidneys in the area of the back near the waistline. Cortisol is responsible for maintaining the body’s energy supply, blood sugar, and control of the body’s reaction to stress.
Danazol. An androgen-like drug used to treat endometriosis.
Dehydroepiandrosterone (DHEA). A hormone naturally made by the adrenal glands. The body turns it into other hormones such as estrogen and testosterone. DHEA sold as a “natural” supplement is made from plant chemicals and is not regulated by the FDA. It often is marketed as an antiaging medication, but its safety and effectiveness are controversial.
Diabetes mellitus. A condition due to a lack of insulin or lack of response to insulin, resulting in glucose (sugar) levels that are too high.
Diazoxide. A medication that is used to lower blood pressure.
Diuretic. An agent that increases the loss of water from the body.
Eflornithine hydrochloride. A chemical that inhibits enzymes that affect hair growth. Available in a facial cream to reduce the growth of unwanted facial hair.
Endocrinologist. A physician who specializes in endocrinology, which is the medical specialty concerned with hormonal secretions and their actions.
Endometrial biopsy. The removal of a small sample of endometrium (lining of the uterus) for microscopic examination.
Endometrium. The lining of the uterus that is shed each month during menstruation. The endometrium provides a nourishing site for the implantation of a fertilized egg (embryo).
Estrogen. Female hormone produced by the ovaries responsible for the development of female sex characteristics. Estrogen is largely responsible for stimulating the uterine lining to thicken during the first half of the menstrual cycle in preparation for ovulation and possible pregnancy. Estrogen also is important for healthy bones and overall health. A small amount of estrogen also is produced in the male when testosterone is converted to estrogen.
Fallopian tubes. A pair of tubes, attached one on each side of the uterus, where sperm and egg meet in normal conception.
Finasteride. A medication that blocks the conversion of testosterone to more active androgens. May be prescribed for enlarged prostate in men and to reduce hair loss associated with male pattern baldness.
Flutamide. Flutamide is an antiandrogen medication that blocks androgen receptors, preventing the actions of androgens. Flutamide is used in the treatment of prostate cancer.
Follicle, hair. A tubular sheath that surrounds the lower part of the hair shaft, supplies the growing hair with nourishment, and gives life to new hairs.
Follicle, ovarian. A fluid-filled sphere located just beneath the surface of the ovary containing an egg (oocyte) and cells that produce hormones. The sphere increases in size and volume during the first half of the menstrual cycle and at ovulation the follicle matures and ruptures, releasing the egg. As the follicle matures, it can be visualized by ultrasound.
Follicle-stimulating hormone (FSH). The pituitary hormone responsible for stimulating the follicle cells around the egg. FSH stimulates egg development and the production of the female hormone estrogen. FSH also can be given as a medication.
GnRH analogs. Synthetic hormones similar to the naturally occurring gonadotropin-releasing hormones (GnRH) produced by the hypothalamus. GnRH analogs, when given in short pulses, stimulate the pituitary gland to produce FSH and LH. However, when given in more prolonged doses, they decrease FSH and LH production by the pituitary, which in turn decreases ovarian hormone production.
Gonadotropins. Naturally occurring hormones include FSH (folliclestimulating hormone), LH (luteinizing hormone), and hCG (human chorionic gonadotropin). In injection form, these gonadotropins can be used for ovulation induction and other fertility treatments. Other gonadotropins include hMG (human menopausal gonadotropin), hFSH (human follicle-stimulating hormone), and rFSH (recombinant folliclestimulating hormone).
HAIR-AN syndrome (hyperandrogenism, insulin resistance, acanthosis nigricans). A genetic disorder associated with very high circulating levels of insulin and androgens.
Hirsutism. The growth of long, coarse hair on the face, chest, upper arms, and upper legs of women in a pattern similar to that of men. Hirsutism may be due to excess levels of androgens.
Hormones. Substances formed in one organ of the body, such as the pituitary or adrenal glands, and carried by a body fluid to another organ or tissue where they have a specific effect.
Hyperandrogenism. A condition in which women have elevated levels of androgens (male hormones).
Laparoscopy. A surgical procedure in which a laparoscope, a thin, lighted viewing instrument with a telescopic lens, is inserted through a small incision in the navel to examine the female reproductive organs and abdominal cavity. Other long, slender instruments may be inserted through additional incisions.
Luteal phase. The second half of the ovarian cycle when the corpus luteum produces large amounts of progesterone. This progesterone is important in preparing the endometrium to receive a fertilized egg (embryo) for implantation.
Luteinizing hormone (LH). The pituitary hormone that triggers ovulation and stimulates the corpus luteum of the ovary to secrete progesterone and estrogen during the second half of the menstrual cycle.
Menstruation. The normal, cyclic shedding of the endometrial lining (lining of the uterus), which appears as a bloody discharge from the uterus.
Minoxidil. A medication used to lower blood pressure that was also found to promote hair growth.
Non-classical adrenal hyperplasia (NCAH). An inherited disorder in which the adrenal glands do not produce enough of the hormone cortisol and overproduce androgens. Elevation of the hormone 17 alphahydroxyprogesterone is characteristic of NCAH. NCAH is a genetic disorder most commonly seen in certain ethnic groups, including Ashkenazi Jews, Eskimos, and French-Canadians.
Ovarian drilling. A laparoscopic procedure, using laser or electrocautery, to destroy the androgen-producing tissue in the ovaries. This procedure is usually a last resort for ovulation induction in PCOS patients who have not responded to hormonal treatments.
Ovaries. The two female sex glands in the pelvis that produce eggs, estrogen, and progesterone.
Ovulation. The release of a mature egg from its follicle in the outer layer of the ovary. This usually occurs approximately 14 days before the next menstrual period (the 14th day of a 28-day cycle).
Phenytoin. An anti-seizure medication.
Pituitary gland. The small gland just beneath the hypothalamus that controls ovarian function by secreting follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Disorders affecting this gland may lead to irregular or absent ovulation.
Polycystic ovary syndrome (PCOS). A condition in which the ovaries contain many cystic follicles associated with chronic anovulation (lack of ovulation) and overproduction of androgens (male hormones). The cystic follicles exist because the eggs are not expelled at the time of ovulation. Symptoms may include irregular menstrual periods, excessive growth of body hair in a male-like pattern (hirsutism), and infertility. Also called polycystic ovarian syndrome and Stein-Leventhal syndrome.
Progesterone. A female hormone secreted by the corpus luteum after ovulation during the second half of the menstrual cycle (luteal phase). It prepares the lining of the uterus (endometrium) for implantation of a fertilized egg and also allows for complete shedding of the endometrium at the time of menstruation.
Spironolactone. A steroid hormone that directly blocks the effect of androgens on the skin. It initially was used as a diuretic or water pill to increase urine output. A brand name is Aldactone®.
Steroids. Hormones that are derived from cholesterol. Categories of steroids include sex steroids (estrogens, androgens, progestogens), glucocorticoids (hormones that closely resemble cortisol), and mineralocorticoids (hormones related to aldosterone and involved in fluid and electrolyte control). Man-made steroids closely resemble cortisol, a hormone naturally produced by the adrenal glands. Steroids decrease inflammation, reduce immune system activity, and are used to treat a variety of inflammatory diseases and conditions.
Terminal hair. The long, coarse, thick hairs that normally grow in the scalp, pubic, and armpit areas of men and women and the face, chest, abdomen, upper arms, and upper thighs of men.
Testes. The two male reproductive glands located in the scrotum that produce testosterone and sperm.
Ultrasound. High-frequency sound waves that produce an image of internal organs on a screen. May be used to monitor growth of ovarian follicles or a fetus. Ultrasound can be performed either abdominally or vaginally.
Uterus. The hollow, muscular organ in which the fetus develops during pregnancy.
Vellus hair. The soft, fine, usually short hairs that appear on the face, chest, and back of women, giving the impression of “hairless” skin.
FIND AN EXPERT
Coping with hirsutism and PCOS can be emotionally challenging. You may feel self-conscious or concerned about issues like excessive hair growth, weight management, or future fertility. It’s important to remember that many people experience similar challenges, and these conditions are more common than you might think. Seeking support early on can make a difference, as early diagnosis and treatment often lead to better outcomes.
Even though you may feel hesitant to share these feelings, talking with a physician can open doors to medical and cosmetic treatments that address both PCOS and hirsutism. A range of options is available, including medication, and, if needed, electrolysis or laser treatments to permanently reduce unwanted hair.
If you’re seeking specialized help, ASRM can assist in finding a reproductive endocrinologist knowledgeable about Polycystic Ovary Syndrome. This specialist can guide you on your journey and help you address your specific goals and concerns.
Search for an Expert
Fact Sheets/Booklets
View more fact sheets and booklets written by the ASRM Patient Education Committee.
Menopausal Transition (Perimenopause): What Is It?
The menopausal transition (perimenopause) is the period that links a woman’s reproductive (childbearing) years and menopause.
Osteoporosis
Osteoporosis and osteopenia are conditions of having low bone mass (density).